Contents
The pancreas is an internal organ that is necessary for the absorption of glucose that enters the human body with food. The gland secretes hormones such as glucagon and insulin, as well as enzymes necessary for the proper digestion of food. Inflammation of this organ is called pancreatitis. If enzymes stagnate in the pancreas itself and do not enter the intestines, they can cause irritation and swelling of the mucous membrane lining the inner surface of this important organ of the digestive system. Inflammation can develop suddenly, or it can drag on for years. And over time, the pancreas is gradually destroyed.
Causes of inflammation of the pancreas

The most common provoking factors leading to pancreatitis are alcohol abuse and gallstones. Also, this disease can develop due to injuries, infections and uncontrolled intake of certain medications. Sometimes it happens that the causes that led to inflammatory processes in the pancreas remain idiopathic (unexplained). In a normal state, the pancreas and its ducts do not allow enzymes to corrode the cells of the mucous membrane. But sometimes the outflow of enzymes into the small intestine fails, and digestive juices begin to have a devastating effect on the tissues of the gland itself.
Acute form of pancreatitis
Most often, an acute attack of pain leads to blockage of the pancreatic ducts by gallstones or excessive alcohol intake. A sudden attack of pancreatitis is also caused by prolonged binges.
Other reasons can also include:
Injuries;
Infections;
Elevated levels of triglycerides in the blood;
Certain medicines (steroids, antibiotics, medicines for the treatment of hypertension).
Chronic form of pancreatitis
Experts believe that the development of chronic pancreatitis leads to excessive passion for fatty foods, smoking and alcohol abuse. It is not exactly clear how alcohol affects the pancreas. Presumably, it can impede the release of digestive juices from the pancreas or greatly change their chemical composition, so they begin to cause an inflammatory process.
Symptoms of inflammation of the pancreas
The most obvious symptom of inflammation of the pancreas is a rather severe pain in the left hypochondrium or in the upper abdomen. Sometimes the pain radiates to the lower back and is girdle in nature. When taking a sitting position or leaning forward slightly, the pain gradually subsides and becomes insignificant.
Also, symptoms include:
Tachycardia (rapid heartbeat);
Nausea and vomiting;
increased sweating;
state of shock;
Yellowing of the whites of the eyes and skin;
Back pain, but this symptom is sometimes provoked by diseases such as peptic ulcer, appendicitis, cholecystitis, intestinal obstruction, diverticulosis.
What happens when the pancreas becomes inflamed?
Acute pancreatitis
Pancreatitis can be mild or severe. The most common diagnosis is acute mild pancreatitis. Such a disease does not affect nearby organs and is cured quickly enough. With the appointment of the correct therapy, the symptoms of the disease disappear a week after the start of treatment.
The therapy is carried out directly in the hospital under the supervision of a doctor who, depending on the individual characteristics of the human body, prescribes painkillers and anti-inflammatory drugs and develops a system for taking them. As soon as the inflammation is eliminated, the patient will immediately recover.
But sometimes pancreatic tissue necrotization or severe damage to its cells can occur. In this case, there is a danger of complete organ failure. In an advanced case, inflammatory processes in the pancreas can lead to death.
Chronic pancreatitis
Usually the disease becomes chronic after a series of attacks of acute pancreatitis and in the absence of adequate treatment. The most likely cause of chronic inflammation experts call the constant abuse of alcoholic beverages.
This form of the disease proceeds in different ways. Often chronic pancreatitis is accompanied by regular pain and associated complications. They include constantly recurring manifestations of all the symptoms of pancreatitis, blockage of blood vessels, small intestine, bile ducts, accumulation of air and fluid.
With the death of most of the tissues of the pancreas, malnutrition occurs, as the body ceases to produce the enzymes necessary for digestion that help digest proteins and fats. The body cannot absorb fats, and they are simply excreted in the stool. It becomes thin, pale and offensive due to the development of steatorrhea.
Damage to the cells responsible for the production of insulin (insulacytes) leads to the inability to absorb carbohydrates and sugar from food, which threatens the development of diabetes. The chronic form of the inflammatory process of the pancreas increases the risk of developing cancer. It occurs in about 4 cases out of 100 in people with chronic pancreatitis.
Risk Factors
The following factors significantly increase the risk of pancreatitis:
Alcohol abuse. It all depends on the individual characteristics of the organism. The amount of alcohol that can lead to the destruction of pancreatic cells varies from person to person. On average, medical experts suggest that men can drink no more than two glasses of strong alcohol per day, and for women this rate should not exceed one glass;
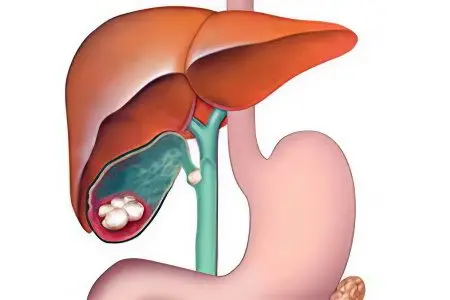
Stones in the gallbladder. Gallstone disease can lead to blockage of the pancreatic duct, and as a result, the outflow of digestive juices will be disturbed;
Elevated levels of triglycerides in the blood;
Deviation in the structure of the bile or pancreatic ducts, and congenital pathology, when the pancreas is divided and has two main channels.
Diagnosis of inflammation of the pancreas
If inflammation of the pancreas is suspected, the following medical specialists can take part in the diagnosis of this disease: a general practitioner, a surgeon, a family doctor, a gastroenterologist. A visual examination is carried out, a blood test is prescribed, which may indicate the presence of blockage of the ducts or their infection. Then other studies are additionally prescribed, including ultrasound, which is the most common painless diagnostic procedure.
Primary examination. First, the doctor conducts a visual examination and asks about the symptoms. Also finds out all the diseases that preceded this health problem. If there is a suspicion of cholelithiasis, then the doctor pays attention to the yellowish tint of the skin and whites of the eyes, conducts a digital examination of the abdomen. If there are attacks of nausea or vomiting, then it is necessary to find out their causes. To do this, you should describe your feelings at the doctor’s appointment as accurately as possible. It is necessary to accurately indicate the number of attacks and their duration. For a more thorough study, detailed blood tests, urine tests, as well as an X-ray examination can be prescribed.
Analyzes. To begin with, a study of the level of enzymes in the blood is prescribed. Based on the results of the data obtained, the doctor diagnoses the disease and decides on the appointment of treatment for inflammation of the pancreas.
To compile a clearer picture, two main blood tests are prescribed:
lipase level. An increase in its level in the blood may indicate an acute attack of pancreatitis;
amylase level. High amylase levels are a sign of inflammation.
Also, in addition to the above tests, you can additionally appoint:
Analysis for bilirubin. An increase in the level of this protein occurs when the bile ducts are blocked;
Complete blood count. If the pancreas is inflamed, then a large number of leukocytes will be present in the blood;
Blood test for liver enzymes. In acute pancreatitis, which is caused by gallstones, there is an increase in the activity of alanine aminotransferase and alkaline phosphatase.
Clinical researches
The following hardware techniques are used:
Ultrasound examination of the abdominal cavity. With its help, you can find out how badly the duct is clogged, and where the gallstones are located;
CT with contrast. With the help of computed tomography with the addition of a contrast agent, other causes of abdominal pain are excluded. Also, this procedure helps to exclude intestinal obstruction, find complications, determine dead tissue (pancreatic necrosis), see blockage of veins;
MRCT (magnetic resonance cholangiopancreatography). Performed to detect gallstones in the common bile duct;
ECHR. Endoscopic retrograde cholangiopancreatography. Allows the specialist to see the structure of the main pancreatic duct. This is the only diagnostic test that can be used simultaneously to remove stones from the common bile duct and to treat narrowed bile ducts;
MRI. This procedure is used to detect inflammation and to complement the information obtained with computed tomography;
Endoscopic ultrasound. This procedure is carried out using a specially designed endoscope, which is inserted through the esophagus directly into the stomach. With the help of this study, the presence of gallstones in the bile ducts is revealed;
Puncture. A similar procedure is prescribed in cases where the specialist is not sure whether there is a process of infection of the pancreatic tissues. The puncture is taken from the inflamed area of the organ. Then the obtained sample of tissue or fluid is examined in the laboratory for the presence of pathogenic microorganisms that cause inflammation. If pancreatitis occurs in a complex chronic form, then it is necessary to analyze the feces for the presence of fats in it. If they are present there, then this will indicate that fats are not digested and absorbed by the body. This means that the pancreas does not secrete enough digestive enzymes.
Treatment of inflammation of the pancreas

Most often, treatment is carried out in a hospital. A sick person is prescribed painkillers, and a special drug regimen is being developed to eliminate inflammation. In pancreatitis, air and fluid sometimes accumulate in the stomach, which can cause severe vomiting. To eliminate this symptom, a tube is inserted into the stomach through the nose, which brings fluid and air out.
The choice of therapy for pancreatitis will depend on the nature of the disease: an acute attack or a chronic course. Initial treatment for an acute attack of pancreatitis should be carried out in a hospital setting. The patient is prescribed intravenous infusions to replenish fluid loss and normalize blood pressure. NSAIDs are prescribed to eliminate inflammation. During this period, from three days to a week, a strict diet is observed.
In the presence of gallstones that provoke attacks of inflammation of the pancreas, ERCP (endoscopic retrograde cholangiopancreatography) is prescribed to remove them from the bile duct. After the elimination of inflammatory processes, sometimes the gallbladder is removed surgically.
In the chronic course of the disease, when acute attacks of pancreatitis appear, a similar treatment is prescribed. If it is necessary to expand the pancreatic ducts, remove stones or cysts, it is necessary to resort to surgical intervention. After such a procedure, a person should be constantly observed by the attending physician for about six months in order to avoid complications. At home, you should constantly adhere to an appropriate diet, avoid overeating and alcoholic beverages.
Drugs for the treatment of chronic inflammation of the pancreas
In the treatment of the chronic form of pancreatitis, painkillers, enzymes that improve the digestion of food, and, if necessary, insulin-containing drugs are prescribed.
The main types of drugs for the treatment of pancreatitis:
Anesthetics. If the pain attacks are tolerable, then they can be stopped with ibuprofen or acetaminophen. With more intense and sharp pains, as prescribed by the doctor, stronger painkillers are used;
Insulin. If inflammation has led to the death of pancreatic cells responsible for the production of insulin, then the patient is prescribed insulin injections for life;
Enzymes With a severe form of inflammatory processes in the pancreas, this organ can stop the production of digestive enzymes, which are vital for the digestion and proper absorption of fats, carbohydrates and proteins. In this case, the patient is prescribed the intake of enzymes. Entering the body, they help food to be fully absorbed.
With caution and under the direct supervision of a physician, enzymes should be taken in childhood, since a large amount of them can lead to intestinal obstruction.
When is surgery necessary?
The pancreas is a very delicate organ that is quite easy to damage during surgery, doctors prefer not to prescribe interventions whenever possible. However, sometimes surgery is simply necessary, since the risk of complications due to dead pancreatic tissue is much higher than the risk of complications of surgical treatment.
If pancreatitis is caused by the presence of gallstones, then two types of operations are usually chosen:
Laparoscopy;
Open surgery on the gallbladder.
In the presence of stones in the gallbladder, endoscopic retrograde cholangiopancreatography is used. It is also resorted to if it is necessary to expand or drain a narrow pancreatic duct.
To eliminate dead tissue of the pancreas, various methods are used:
Laparoscopic necrectomy, which is performed with limited necrosis of the pancreatic tissue. Such an operation is important for saving the patient’s life, although after it the volume of enzymes and hormones secreted by the body decreases;
Open necrectomy. It is indicated for the extensive distribution of necrotic processes in the tissues of the pancreas. Excision of necrotic cells is carried out, followed by removal of inflammatory exudate, drainage of retroperitoneal tissue and lavage of purulent cavities.
necrectomy pancreas This is an organ-sparing operation that involves the removal of all dead tissue.
What to do if complications of the inflammatory process begin?

Attacks of pancreatitis do not pass without a trace and are often accompanied by complications. These include:
Necrotization of pancreatic tissue;
Infection;
Cyst.
Sometimes surgery is required to remove stones from the gallbladder or resection of the damaged part of the pancreas. If the violations are critical, then the patient will most likely have to take insulin to regulate blood sugar levels. And for the normal digestion of proteins and fats, drugs are prescribed that contain digestive enzymes.
If the inflammation of the pancreas is chronic, then the sick person needs to follow a constant diet, which completely excludes the consumption of alcoholic beverages, including low-alcohol ones. It is also necessary to constantly take painkillers. The patient needs to develop a nutrition system together with the attending physician. Changing your eating habits is quite difficult, especially for people with a weak will, but with the right approach, good planning and family support, all this becomes possible.
Complications of chronic pancreatitis include:
Accumulation of excess fluid around the pancreas;
blockage of blood vessels;
Constant bouts of pain;
Stenosis of the bile ducts and small intestine;
The risk of developing pancreatic cancer.
Treatment when the patient’s condition worsens
The consequence of a long chronic inflammation of the pancreas is a decrease in the amount of digestive enzymes secreted by it. Therefore, the body cannot fully digest fats. Decreased synthesis of enzymes leads to steatorrhea. This is a liquid, oily stool.
Since proteins and fats are not absorbed from food, a person begins to lose weight. Solve this problem with the help of medicines containing enzymes. If pancreatitis has led to the cessation of secretion of the hormone insulin by the pancreas, then appropriate injections are prescribed to the sick person.
In the course of treatment, with the development of an infectious inflammatory process, the patient is prescribed antibiotics or the necrotic affected pancreatic tissues are surgically removed. However, doctors try to treat this organ without resorting to surgical intervention, since the pancreas is very delicate and vulnerable.
Prevention of inflammation of the pancreas

Guaranteed to prevent inflammation of the pancreas, like any other disease, is impossible.
However, you can reduce risk factors and thereby minimize the likelihood of new seizures:
Since most often attacks of pancreatitis occur against the background of the abuse of alcoholic beverages, then in the presence of such a disease, alcohol should be completely excluded from your life. Even a small amount of it can provoke an attack of pain or complications. Large doses of alcohol can be life-threatening for a person with pancreatitis;
Since chronic pancreatitis is accompanied by bouts of pain, painkillers are prescribed, as well as digestive enzymes;
The intake of fatty, fried, smoked, spicy foods is limited, as they irritate the pancreas and cause pain;
If pancreatitis is provoked by gallstones, then you should monitor your diet and lead a healthy, active lifestyle;
Smoking also provokes the development of pancreatic diseases, so you should think about quitting this bad habit;
In food, you need to eat more fresh fruits and vegetables, lean meats, baked goods made from wholemeal flour, cereals cooked in water.
Only a timely visit to a doctor in the presence of the first symptoms of pancreatitis, compliance with all his recommendations for the treatment and prevention of the disease, will help maintain the normal functions of such an indispensable digestive organ as the pancreas.
Whom should I contact?
To diagnose inflammation and treat inflammation of the pancreas can:
Family doctor;
local therapist;
Gastroenterologist (specialist in diseases of the gastrointestinal tract);
Abdominal surgeon.










پیٹ کا سرجن