Contents
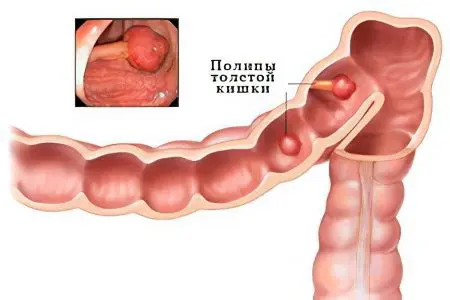
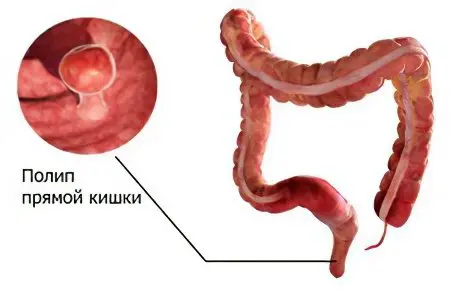
A polyp in the rectum is an epithelial formation of benign origin and originating from the mucous membrane of the anorectal region. It grows into the intestinal lumen and is recognized by doctors as a precancerous condition. Such growths can be single and multiple, can be combined into groups. Sometimes rectal polyposis is diagnosed even in childhood.
As for the form of such neoplasms, four varieties of them can be found: a polyp has either the appearance of a mushroom (under it there is a thick or thin leg), or it looks like a bunch of grapes, a sponge or a dense knot.
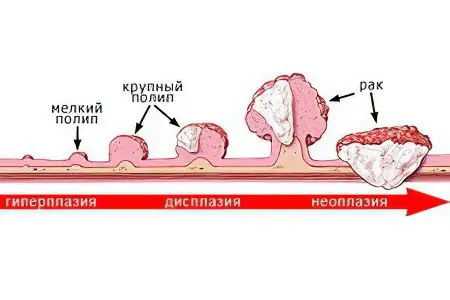
Despite the fact that the frequency of detection of polyps during sigmoidoscopy does not exceed 7,5%, they are much more common. The errors of the available statistics are quite understandable, and are primarily due to the asymptomatic course of the disease. In addition, there is evidence that at autopsy, polyps in the rectum are found in 30% of the dead.
Those people who have crossed the age limit of 45 years should definitely undergo a colonoscopy for preventive purposes, since polyps are found in 10% of cases in adult patients. At the same time, 1% of patients are carriers of malignant tumors. And the more polyps, the higher the risk of their malignancy.
Symptoms of polyps in the rectum
It is rather difficult to suspect a polyp by symptoms, since the clinical signs are nonspecific and may indicate many other intestinal pathologies.
However, the following manifestations should be the reason for an immediate appeal to the doctor:
Feeling of discomfort, as well as the feeling of a foreign object in the anus. Most often, this symptom indicates the presence of education in the rectum. Similar feelings arise in response to the pressure of the tumor on the opposite wall of the intestine. However, a pronounced feeling of discomfort appears only when the outgrowth reaches a large size. The patient does not experience the sensation of a foreign object on an ongoing basis. An unpleasant feeling occurs periodically and is cramp-like in nature. In addition, discomfort may appear in the pubic area or on the side. If the pathology has progressed, then the pains can disturb a person constantly, they change their character and become bursting;
Pain in the lower abdomen. Pain is never a companion of young polyps, negative sensations appear as the disease progresses. A painful reaction is the response of the receptors of the rectum and large intestine to existing congestion. After all, the larger the neoplasm, the narrower the intestinal lumen, as a result, the exit of feces in a natural way is very difficult. A sick person suffers from regular prolonged constipation. The constant presence of feces in the intestine stretches its loops, which in turn causes pain. In addition, pain in the lower abdomen can be triggered by increased gas formation;
Violation of the stool, manifested in diarrhea and constipation. This symptom is an early manifestation of polyps. More often, patients suffer from constipation, which occurs due to a mechanical barrier in the form of a polyp. If in the early stages constipation can alternate with diarrhea, then the larger the polyp becomes, the less often diarrhea occurs. The chair can be observed no more than twice a week. The duration of its absence depends on the number of polyps present. It often happens that it is a long delay in stool that forces a person to come for a consultation with a doctor;
The presence of mucous contents and blood in the stool. The blood that stands out from the anus and is visible to the naked eye is a formidable symptom. It often indicates damage to the blood vessels of the submucosal layer of the rectum. In addition, blood can signal a pinched polyp or its necrosis. To detect blood, you need to look at the feces, it is most often found on their surface and looks like red streaks. Mucus is a constant companion of polyps in the intestines. The fact is that the formations have an increased excretory function. Normally, mucus is needed to lubricate the rectum, which makes the passage of feces through it more comfortable. However, the polyp irritates the intestinal walls and additionally stimulates the excretory glands. When mucus accumulates in the anal sinuses and remains there for a long time, it can provoke an infection. In this case, in a patient after prolonged constipation, stool will be excreted along with mucous and even purulent contents.
The clinical picture of the disease may vary somewhat. It depends on the histological structure of the formation itself.
The clinical picture of the disease may vary somewhat. It depends on the histological structure of the formation itself. Distinguish:
Adenomas or glandular polyps. It is with such neoplasms that bleeding is rarely observed, which is associated with their infrequent ulceration. They are dense and have a pinkish tint in tone with the intestinal mucosa. Despite the fact that bleeding with such polyps is rare, they are most often malignantly degenerated. The adenomas are 20 to 30 mm in size. The method of connection with the rectum is different – both a thick and a thin leg can be observed;
Villous polyps, like adenomas, are formed from epithelial tissues. It is with this type of formation that the patient most often experiences rectal bleeding. This is due to the peculiarities of their structure, because they are penetrated by blood vessels. In addition, villous polyps are more likely than others to necrosis and ulceration. Due to the impressive size of the outgrowths (up to 30 mm or more), the patient often suffers from constipation;
Hyperplastic polypswhich do not exceed 5 mm in diameter. They are soft and do not rise too much above the mucous membrane of the rectum. Such neoplasms most often grow absolutely asymptomatically;
Glandular villous polyps have a combined structure. They are observed in 20% of patients and can give only very poor symptoms. Bleeding is rarely observed with such formations, most often blood particles are invisible to the naked eye. It is possible to detect blood impurities in feces only in laboratory conditions.
Causes of polyps in the rectum
Numerous studies designed to establish the cause of the appearance of such polyps indicate that this disease is multifactorial. In addition, it has been established that a healthy intestinal mucosa is an environment in which polyps do not form. Therefore, if the growths were diagnosed, it means that the intestinal lining has undergone pathological changes.
Risk factors include:
Burdened heredity. The development of neoplasms in the rectum is greatly influenced by the patient’s genetic predisposition to intestinal polyposis. When only one person in the family suffered from this disease, the risk of finding such neoplasms in offspring increases several times. Conducted studies indicate that polyps are formed in blood relatives 10 times more often than in the general population. Do not ignore the antenatal factor. At the moment when the walls of the rectum are formed in the fetus, certain disorders occur. Then, as a person grows older, they begin to worsen under the influence of various provoking factors and eventually lead to the formation of polyps;
Eating disorders and prolonged constipation. Excessive content of animal fats in food negatively affects the state of the digestive system in general, and the condition of the rectum in particular. Such products have very little fiber, which is necessary for the normal formation of feces. The refining process goes through many ready-made dishes, the frequency of which should be reduced. The most harmful are chips, carbonated sweet water, smoked meat and fish, products made from white flour, margarine and sugar. Of course, this is not a complete list of products that impair intestinal motility. Including them in your diet in large volumes, the person himself contributes to the fact that the feces remain in the intestines for a long time. As a result – prolonged constipation and aggravation of the risk of developing polyps. Canned foods, as well as canned carbonated drinks, additionally have a negative effect on the intestinal mucosa. For example, the potentially toxic Bisphenol A used in tin packaging can be found in varnishes, plastics, and other non-food products. Also, excessive consumption of palm oil, rich in trans fats, and alcoholic beverages will not bring benefits to the intestines;
Chronic intestinal pathologies. Diseases that can provoke the development of polyps are colitis, proctosigmoiditis and ulcerative colitis. Each of them, with a long course, contributes to dangerous changes in the rectal mucosa and the growth of neoplasms;
Acute intestinal infections. During the infectious process, the large intestine is affected first of all. This further becomes a prerequisite for the formation of polyps in the rectum. The danger is represented by diseases such as rotavirus infection, salmonellosis, dysentery. Even if it is possible to get rid of the disease quickly enough, each of these infections leaves its own “imprint” on the intestinal mucosa. As a result of inflammation and oxygen deficiency, structural changes occur in the epithelial tissues of the intestine, where polyps subsequently develop;
Hypodynamia and poor environmental conditions. These are two rather relevant factors for modern people. Sedentary work provokes stagnation of blood in the small pelvis, resulting in violations of the venous and lymphatic outflow. This contributes to tissue swelling, which, together with chronic constipation, stimulates the growth of polyps.
Why are polyps in the rectum dangerous?
Such neoplasms pose a real threat to human health and life. There are several dangers:
The transformation of a polyp into a cancerous tumor. Of particular danger in this regard are adenomas, which are diagnosed most often. A subtype of adenomas is villous adenomatous polyps, which have multiple finger-like processes. It is they who malignize more often than others. The risk of malignant degeneration is significantly increased with extensive polyp growth, as well as with a wide base. Such adenomas are more aggressive, since the absence of a stem contributes to the accelerated migration of malignant cells to adjacent structures;
Development of intestinal obstruction. In the presence of a large rectal polyp, the feces stagnate. This leads to intoxication of the body, to its dehydration as a result of electrolyte imbalance. If the patient is not provided with adequate medical care, obstruction threatens with the development of necrosis of the intestinal tissues. The consequence will be the ingress of fecal contents into the abdominal cavity, the development of peritonitis and the death of the patient;
Acute enterocolitis develops against the background of a constantly irritated intestinal wall. Ulcers form on it, they become inflamed, the process captures all parts of the intestine, including the rectum. The patient suddenly begins to experience pain, he is sick, vomits, body temperature rises, blood is found in the feces. If such a person is not provided with medical care in time, he may die due to perforation of the intestinal walls and the development of blood poisoning;
Paraproctitis. Lack of adequate treatment of the polyp can lead to inflammation. An infection from the rectum penetrates into fatty tissue, where a purulent sac is formed. It can be located both inside the adipose tissue and outside. The person begins to suffer from pain, the body temperature rises. When the disease passes into a chronic form, the patient’s ability to work is impaired, he becomes lethargic, gets tired faster;
Stool disorders, which are manifested in the alternation of constipation and diarrhea. With adenomatous formations, patients often suffer from watery diarrhea, which is due to the abundant release of salt and water by the polyp itself. Due to the leaching of potassium, a person develops hypokalemia, which affects all body systems in a negative way. The inability to contain gases and feces is a frequent unpleasant complication of polyps located near the entrance to the anus;
The formation of fecal stones. If the feces are in the intestines for a long time, this can lead to their hardening and the formation of stones. Such round seals disrupt the digestive system, reduce immune defenses, lead to intoxication of the body, cause discomfort and pain in the abdomen;
Fissures in the rectum. They are formed due to the difficult act of defecation, since a sick person has to strain the muscles of the anal canal all the time. Cracks deliver particular pain during an attempt to empty, often provoke mild bleeding, and sometimes can cause suppuration. Against the background of constant discomfort when trying to empty the intestines, a person begins to fear each subsequent act of defecation and unconsciously try to delay it. This leads to the formation of constipation and fecal stones;
Anemia – Another threat posed by polyps. At the same time, the patient, against the background of constant blood loss, experiences fatigue, weakness, loss of strength.
Diagnostics
Diagnosis in case of suspicion of this pathology includes the following types of studies:
Palpation of the anorectal region. A similar technique for suspected polyposis of the rectum is used in the first place. Finger research makes it possible to feel the rectum for 100 mm from the entrance to the anus. If in the future it is planned to conduct sigmoidoscopy, then preliminary palpation is still mandatory. It allows you to assess the condition of the sphincters and mucous membranes, suggest the presence of a polyp. After the examination is completed, a decision is made on the need for further diagnostics;
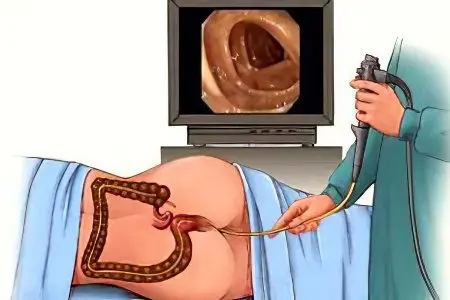
Rectoromanoscopy. The procedure allows you to determine the condition of the mucous membranes of the rectum and the beginning of the colon. It is realized with the help of a rectoscope. Allows you to examine the intestines during the first 30 cm. To straighten the folds of the intestine, the doctor uses a special airflow. There are some contraindications to the procedure. Among them, the narrowing of the intestinal lumen, severe rectal bleeding, intestinal disease in the acute phase, anal fissures. In order for the procedure to be as comfortable as possible for the patient and give as much information as possible, it is necessary to properly prepare the patient. This requires cleansing enemas with boiled water, which are done according to the schedule agreed with the doctor;
Irrigoscopy. This diagnostic method is used somewhat less frequently than sigmoidoscopy. It comes down to the introduction of a contrast agent into the intestinal cavity. It is well visualized under the influence of X-rays, which also allows you to see the walls of the intestine. This method requires the patient to prepare in advance. For irrigoscopy, the patient’s intestines must be completely empty, so you must first make an enema with boiled water. Take a laxative in the evening. Dinner should not consist of foods that take a long time to digest. It is important to exclude foods that increase gas formation from the diet a few days before the study. This applies to coffee, beans and cabbage. You can not have breakfast in the morning before the procedure;
CT scan. This diagnostic method is the most painless for the patient, and also provides reliable information about the condition, shape and size of polyps without penetrating into the intestine;
Laboratory research. To confirm the diagnosis, the patient must donate blood for biochemical and general analysis. By themselves, these methods will not give the doctor the opportunity to make an unambiguous diagnosis. However, they are able to complete the picture of the disease. So, with prolonged bleeding, a decrease in the amount of hemoglobin will be noticeable, which is a sign indicating anemia. In addition, the feces are examined to detect latent blood, particles of undigested food and mucus in it. Often a coprogram makes it possible to determine the etiology of a pathological formation, because from its results it can be seen whether the patient suffers from dysbacteriosis.
Answers to popular questions
Do I need to remove polyps in the rectum? Such neoplasms after their diagnosis are subject to mandatory removal. Otherwise, you risk getting the complications described above.
How long does the rectum heal after polyp removal? The recovery period can take up to three months. It all depends on the scope of the operation. As a rule, the wound itself heals two weeks after the removal of the polyp.
Treatment of polyps in the rectum
Conservative therapy is not used when such a pathology is detected. No drug can eliminate a polyp from the body or make it smaller. However, sometimes medications may be prescribed to the patient before surgery. They are aimed at relieving pain or eliminating increased gas formation.
Removal of polyps in the rectum
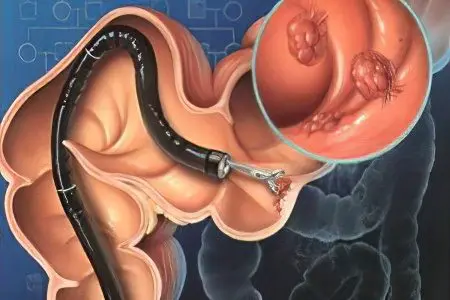
Surgical intervention is the only method that allows you to remove pathological growths of the rectal mucosa. Depending on the type of polyps and how many there are, either a full-fledged operation or an endoscopic procedure will be prescribed.
Electrocoagulation
The patient must be prepared before the procedure. To do this, he is assigned several enemas to cleanse the intestines. 12 hours before the start of the cauterization procedure, you must refrain from eating. Special laxatives, such as Mucofalk, may also be prescribed.
Electrocoagulation of rectal polyps can not be performed in all cases. The operation allows you to save the patient only from single formations located no further than 30 cm from the entrance to the anus, but no closer than 10 cm from it. In addition, there should be no signs of a malignant process, and the polyp itself should not be less than 10 mm or more than 30 mm in size.
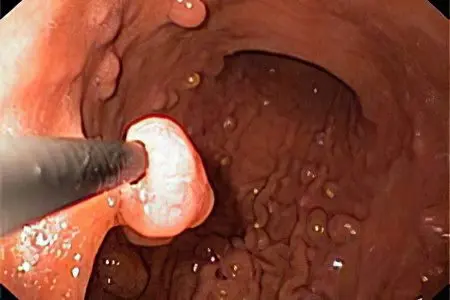
During the procedure, a rectoscope is inserted into the intestinal cavity, after examining the neoplasm, the doctor brings a diathermic loop to it. With it, the doctor captures the tumor by the leg, after which the polyp is coagulated with the help of a high-frequency current, and then it is removed from the intestine.
If the polyp is small (up to 3 mm), then fulguration can be applied. In this case, the formation is touched once, as a result of which the polyp is burned. However, with this procedure there is a risk of perforation of the intestinal wall.
Transanal excision
If villous and adenomatous polyps are found in the rectum, which are located at a close distance from the beginning of the anal canal, then transanal excision is indicated. Preparation for the procedure is to conduct cleansing enemas.
Before the start of the operation, the patient is given anesthesia. For this, Novocaine 0,25% is used. After the onset of the drug, a rectal speculum is inserted into the anus.
When the polyp holds on to the intestinal wall with a small leg, the doctor crosses it directly near the base. When the bed of the polyp is wide, then its oval excision is performed. The resulting wound is treated with an antiseptic.
Among the disadvantages of this intervention, mainly, there is a high probability of bleeding. To prevent it, either suturing or subsequent electrocoagulation of the vessels is necessary. After 3 months, the patient must undergo a control sigmoidoscopy.
Transanal endoscopic microsurgery
In this case, a proctoscope is used to remove the neoplasm from the rectum. It is equipped with equipment for blowing the intestinal wall, a camera and lighting. The polyp is removed using specialized instrumental equipment. This method has a number of advantages, including the removal of polyps from any part of the rectum, the ability to prevent bleeding by instant coagulation, resection of growths not in parts, but in whole.
Electroexcision
To carry out this intervention, an electric loop is required, it is with its help that the neoplasm is removed. When it is thrown over the polyp, the doctor will apply current, the loop will heat up and destroy the polyposis tissues. The cells die, then the doctor will tighten the loop and cut off the formation.
It is important that during this procedure there is an instant coagulation of the vessels, which means that bleeding will not occur. This is especially true when removing polyps from the rectum, since most of them have a developed circulatory network. Therefore, the development of rectal bleeding is often a complication that appears after resection.
Removal of polyps with a laser
The mass can be removed from the rectum using a laser. This can be cauterization or excision with a laser beam. Like any other operation, this type of intervention requires the preparation of the patient. Laser cauterization cannot be performed in the presence of large polyps, since the risk of perforation of the intestinal wall increases significantly. Also, using this technique, villous formations are not eliminated. The procedure does not require general anesthesia and is performed under visual control. Coagulation is performed in stages, which reduces the trauma of the procedure. In parallel with the evaporation of pathological cells, the vessels are sealed. This contributes to the fact that bleeding, as a complication of the operation, does not occur.
Laser excision is possible with villous polyps. However, they should be located no further than 80 mm from the entrance to the anus. Local anesthesia is also used for anesthesia. The advantage of this method, in addition to the absence of bleeding, is also the fact that the treated area is disinfected using high temperatures. This ensures that there will be no infectious complications after treatment. To minimize the chance of recurrence, the attachment site of the growths is also coagulated. The procedure itself is quite fast and does not take more than 20 minutes.
Resection of the rectum
If at the diagnostic stage signs of malignancy of formations were found, then a radical method of surgical treatment is used – resection. It consists in removing the rectum along with existing polyps. Also, the intestine can be cut out partially, then the surgeons talk about extirpation. The procedure will require general anesthesia.
If a polyp is found in the lower or middle lobe of the rectum, the doctor performs a lower anterior resection. When anesthesia begins to take effect, the surgeon makes an incision in the abdominal wall, located in the lower abdomen. Then it directly removes part of the intestine. The volume of the excised part directly depends on the size of the malignant formation and the degree of development of the oncological process. If the degeneration has already occurred, and the cancer cells have penetrated into nearby tissues, then complete removal of the rectum is required. When doctors detect metastases, in addition to the rectum, lymphatic vessels located nearby are removed from the body. After performing a total resection, the remaining free end of the ileum is connected to the anus.
As for the prognosis for recovery, it is favorable subject to timely detection and competent treatment. Relapses can be observed, they make up no more than 30% of cases. Most often, re-growth occurs after a year. Therefore, a control colonoscopy is so important, which must be carried out 12 months after surgery. If its result is negative, then re-diagnosis should be carried out no less than five years later. The optimal period is 3 years. This is due to the lack of specific preventive measures to prevent the recurrence of the disease.









