Contents
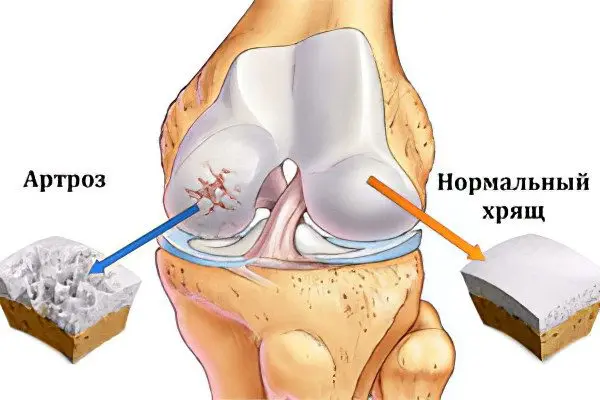
Arthrosis is a disease of the joints, considered dystrophic and associated with the slow destruction of cartilage inside the joint. With arthrosis, over a long period of time, changes occur, restructuring of the articular ends of the bones, inflammatory processes occur, and degeneration of the periarticular tissues occurs. Such a concept as “arthrosis” also includes a not very large group of articular diseases of a degenerative-inflammatory nature, which have different causes and similar mechanisms of their development.
The likelihood of developing osteoarthritis increases many times over with age. The disease equally affects both men and women, the only exception is arthrosis of the interphalangeal joints, since it is most often seen in women. Osteoarthritis overtakes people of working age – from 30 years old, and every year the number of cases is steadily and steadily increasing.
Causes of arthrosis
Osteoarthritis develops due to a metabolic disorder in the joint, which in turn leads to the fact that the cartilage begins to lose elasticity. This can be facilitated by a complete or partial loss of proteoglycans from the composition of the cartilage, this usually occurs due to rather deep cracks in the cartilage itself. The loss of proteoglycans can also occur for another reason: due to the failure of their production by the cells of the joint.
According to experts, the reasons why articular cartilage can begin to break down can be metabolic disorders, hormonal disorders, decreased blood flow to the joint, a hereditary factor, old age, injuries, as well as diseases such as rheumatoid arthritis and even psoriasis. And yet, the most common cause of arthrosis is an abnormal load on the joints, while cartilage cannot resist it.
In addition, the following causes may affect the occurrence and development of arthrosis:
Past trauma. These can be dislocations, bruises, fractures, torn ligaments and other injuries.
Metabolic disorders.
Excess body weight, leading to additional stress on the joints.
Inflammatory process in the joints – acute purulent arthritis.
Elderly age.
Low quality food.
Subcooling.
Autoimmune diseases – lupus erythematosus, rheumatoid arthritis.
General intoxication of the body.
Frequent colds.
Specific inflammations – syphilis, tuberculosis, tick-borne encephalitis, gonorrhea.
Diseases of the thyroid gland.
Blood clotting disorder (hemophilia).
Perthes disease is a violation of the blood supply to the head of the femur.
There are also several genetically determined causes leading to the development of arthrosis:
If we consider arthrosis of the hand and fingers, then scientists have found that the so-called Bouchard and Heberden’s nodules, as a disease, can be inherited.
Violation of the formation of joints and ligamentous apparatus in the prenatal period, which led to dysplasia. Against its background, there is a rapid wear of the joint and arthrosis develops.
Type 2 collagen mutations. When disturbances occur in the structure of the fibrillar protein located in the connective tissue, then there is a rapid destruction of the cartilage.
Also at risk of getting such a disease as arthrosis in the near future are people whose professions are: a bricklayer, a miner, a fisherman, a blacksmith, a metallurgist – and other areas of activity associated with increased physical labor.
Symptoms of arthrosis

A symptom of arthrosis is pain when the joint is loaded, which subsides when the joint is at rest; decreased mobility of the joint, crunch, feeling of muscle tension in the joint area. A joint that is periodically affected by arthrosis can swell, and eventually deform.
Consider the following 4 large groups of symptoms of arthrosis:
Pain. The presence of pain is the first sign of arthrosis of the joints. It can be assumed that with any of their injuries, similar sensations arise, but with arthrosis, pain has some features. Firstly, this is the occurrence of sharp pains or significant discomfort during movement. It will be localized in the place where the diseased joint is located. When a person stops moving and goes into a state of rest, the pain goes away.
At night, a person practically does not experience any discomfort, except during torso flips, having found the optimal position, the patient falls asleep calmly. Pain appears during rest only at the stage of progression of the disease, they have a certain similarity with dental lumbago, when a person cannot fall asleep. They manifest themselves closer to the morning – by 5 o’clock.
So, at the beginning there is practically no pain, it can only be felt during exercise or palpation, over time, human suffering intensifies, and the joint needs more and more periods of rest. Then life completely turns into torture – the hyaline cartilage becomes thinner, the bone is exposed, osteophytes begin to grow. Acute pains torment almost incessantly, even more intensifying in bad weather and the full moon.
Crunch. No less significant symptom of arthrosis is the presence of a crunch. It becomes audible due to the fact that the softness of the rotation of the bones in the joint is reduced, they rub against each other, as a result of which a characteristic sound occurs. The crunch can be heard in other diseases, and even when the joints are healthy. But it is the arthrotic crunch that is distinguished by its “dry” sound. The more the disease progresses, the brighter the sound becomes. At the same time, if a crunch is heard, then pain will also be felt. This is what makes it possible to distinguish the sound made by the joints with arthrosis from the usual harmless clicking.
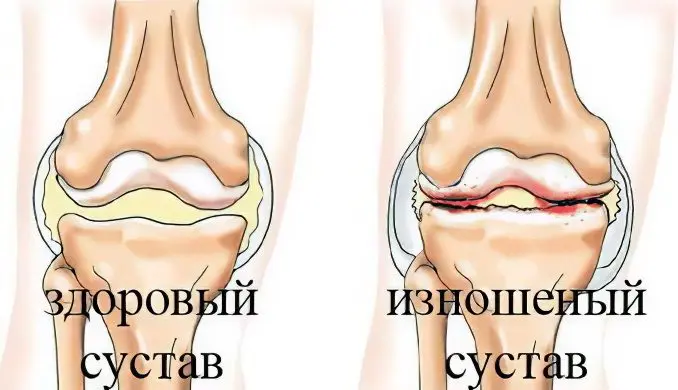
Decreased mobility in the joints This is another characteristic symptom of osteoarthritis. At the initial stage, this phenomenon does not bother the patient, but with the progression of arthrosis, the germination of bone neoplasms leads to the fact that the muscles spasm, and the joint space almost completely disappears. This is the reason for the immobility of the limbs at the site of the lesion.
Joint deformity. Its modification is due to the fact that osteophytes grow on the surface of the bones and synovial fluid arrives. Although deformity is one of the latest symptoms, when arthrosis has already affected the joint to a large extent.
The course of the disease is characterized by stages of exacerbation and stages of remission. This significantly complicates the self-diagnosis of arthrosis, relying only on one’s own feelings. Therefore, it is necessary to consult a doctor for clarification of the diagnosis.
When conducting an x-ray study, he will be able to detect the following signs, allowing to determine the degree of progression of the disease:
Stage 1 is characterized by the absence of osteophytes, the joint space may be somewhat narrowed.
At stage 2, there is a suspicion of a slight narrowing of the gap, osteophytes have already formed.
At stage 3, the narrowing of the gap is clearly visible, there are multiple osteophytes, the joint begins to deform.
Stage 4 is characterized by the almost complete absence of the joint space, multiple osteophytes, and significant deformity.

Degrees of arthrosis
Arthrosis is characterized by degenerative-dystrophic changes in the joints that will haunt a person in the form of a chronic disease. The result of such destruction is damage to the cartilage of the joint, pathological changes in its capsule and synovial membrane, in ligaments and bone structures.
It is customary to distinguish three degrees of arthrosis, which characterize the different severity of the course of the disease and have different symptoms.

1 degree arthrosis
At the first stage of development of arthrosis, serious changes in the morphology of the joint are not observed. Only the composition of the synovial fluid is disturbed. It supplies the articular tissue with nutrients worse, so the cartilage loses its former resistance to the usual loads. This leads to the fact that the cartilage tissues become inflamed, the person has pain.
The patient may complain of slight stiffness in the joints, but most often he does not pay any attention to this feeling, attributing such a health disorder to weather changes, uncomfortable posture, etc.
Sometimes a slight crunch can be heard in the area of the affected joint. Pain is manifested by slight tingling, or may be aching. If the disease is diagnosed at this stage, then it will be possible to cope with it by conservative methods.
2 degree arthrosis
The second stage of arthrosis is accompanied by the destruction of cartilage tissue. Bone growths appear along the edges of the joint. The more intense the load, the more the cartilage tissue of the joint will be destroyed.
A person experiences constant pain to which he gets used. The inflammation then subsides, then again worsens.
The muscles surrounding the joints will lose their former function, but most often such violations are weak or moderate. Therefore, at this stage, a person may refuse to visit a doctor.
After a short load on the legs, a person may experience fatigue. At the same time, aching pain in the joints becomes acute. The crunch increases during movement, which is explained by bone growths.
It is at the second degree of development of arthrosis in the joints that the deforming process begins, so you must definitely seek medical help.
3 degree arthrosis
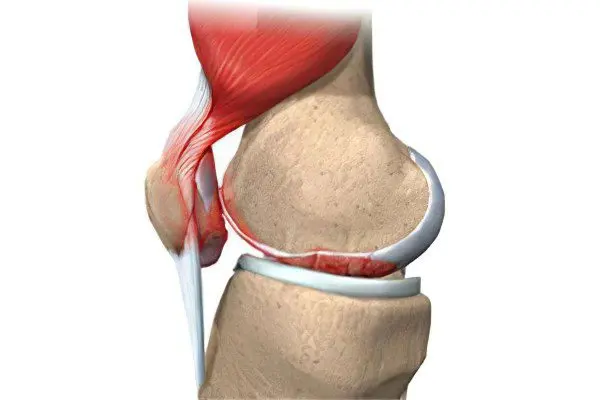
The third degree of arthrosis is the most severe. The articular cartilage of the affected joint is not only thinned, but also began to collapse, and the pathological foci are already quite large. The joint is severely deformed, which affects the normal axis of the limb.
The ligaments that previously surrounded the joint lose their functional activity, become short, which affects the mobility of the arm or leg.
During this period, a person has contractures and subluxations. The muscles surrounding the joint are shortened and stretched, and they contract with difficulty. The joint itself and adjacent tissues suffer from malnutrition.
A person suffers from severe pain, it is sharp and sharp. Even at rest, the patient experiences significant discomfort. The third degree of arthrosis is associated with the risk of complete loss of human capacity.
Types of arthrosis

Depending on the cause of arthrosis, a disease with an unexplained etiology is distinguished, that is, idiopathic arthrosis. It is most often diagnosed in people over 40 years of age. Secondary arthrosis is also distinguished, which occurs against the background of obvious causes (after an injury, with inflammation of the joints, with endocrine diseases, etc.).
In addition to the fact that arthrosis is classified depending on the cause of its occurrence, the following types of the disease are distinguished:
Knee arthrosis or gonarthrosis. This is the most common type of the disease. In this case, it is the knee joints that suffer. Pathology is diagnosed most often in overweight people, against the background of metabolic disorders in the body, and also due to stress. The disease develops over many years, at its late stage, the knee completely loses its mobility.
Ankle arthrosis. With this type of disease, the ankle joint is affected. The disease develops against the background of injuries, with sprains, due to existing dysplasia, gout, diabetes. Sometimes the cause of the pathology is rheumatoid arthritis. Most often, ankle arthrosis is diagnosed in people whose work is associated with excessive stress on this area: dancers, athletes, women who wear high-heeled shoes.
Shoulder arthrosis. The main cause of the pathology is considered to be congenital defects of the shoulder joint, or excessive loads on it. The risk group includes painters, plasterers and people who are engaged in heavy manual labor. This also includes arthrosis of the elbow joint.
Arthrosis of the hip joint or coxarthrosis. This is one of the most severe types of pathology. The main reason is considered to be age-related changes in the articular tissues. The risk group includes people over 40 years of age.
Cervical arthrosis or uncoarthrosis. The reasons that can lead to the development of this pathology: insufficient mobility of the cervical spine, obesity and previous injuries. The risk group includes people who are engaged in sedentary work. In addition to the main symptoms of arthrosis in the form of pain and limited joint mobility, patients experience dizziness, headaches, and sometimes even loss of consciousness. This is due to the involvement in the pathological process of the vertebral artery, which feeds the brain.
Osteoarthritis of the hands and fingers. In this case, the wrist joint, interphalangeal joints, etc. are damaged. Most often, women who have entered the menopause suffer from pathology.
Spondylarthrosis in which the joints and cartilage of the spine suffer. The disease develops most often in people over the age of 65 years. Predominantly women suffer from spondyloarthrosis, which is explained by a decrease in estrogen levels after menopause. Spondylarthrosis can be ankylosing, deforming, facet, polysigmentary and degenerative.
Polyosteoarthritis or Kellgren’s disease. This is a disease of a degenerative nature, in which peripheral joints, ligaments and tendons suffer. The pathology may involve the joints of the spine with the development of discopathy.
Complications of arthrosis
If arthrosis is not given due attention, not treated in time and correctly, this can lead not only to the complete destruction of the diseased joint, but also to a change in the biomechanics of the spine, which may cause hernias in the intervertebral discs and the development of arthrosis in other, still healthy joints. . It is better not to allow a complication of arthrosis of the joints.
The following pathologies are distinguished as the main complications of arthrosis:
Joint destruction.
Joint deformity.
Impossibility of movement.
Patient’s disability.
Violation of the biomechanics of the spine and other joints.
Hernias of intervertebral disks.
Decrease in the patient’s standard of living.
Diagnosis of arthrosis

To make a diagnosis, the doctor must interview and examine the patient. Then he will assign him an x-ray of the affected joints.
X-ray images are performed most often in 2 projections. The study allows you to visualize dystrophic changes in tissues, damage to cartilage and adjacent bones. The joint space in patients with arthrosis narrows, the platform of the bone is deformed, bone growths, osteophytes can depart from it. Sometimes the joint itself loses stability, leading to subluxations.
The first sign of arthrosis that can be visualized on an x-ray is the presence of osteophytes. At first, the edges of the articular surface simply become sharp. In the future, they thicken, and then outgrowths and spikes appear on them. The joint space becomes narrower as the pathology progresses.
Depending on the obtained x-ray picture, the doctor can make the following diagnosis (the classification is taken as the basis Kellgren-Lawrence):
Arthrosis is questionable. It is not possible to determine the degree of narrowing of the joint space, but small osteophytes are visible.
Mild arthrosis, in which osteophytes are well visualized, but there are doubts about the narrowing of the joint space.
Moderate arthrosis is diagnosed when the joint space is clearly narrowed and osteophytes are clearly visible. Sometimes bone deformities are found.
Severe arthrosis is accompanied by a significant narrowing of the joint space and the formation of large osteophytes. The joint will be deformed.
If the doctor needs more information about the condition of the joint, he can refer the patient to undergo a CT scan, arthroscopy, or MRI. To assess the quality of the synovial fluid, an articular puncture is performed.
Therapies

It is better to treat diseased joints at an early stage, the treatment itself should be pathogenetic and complex. The essence of treatment is to remove the causes that contribute to the development of this disease, it is also necessary to eliminate inflammatory changes and restore functions that were previously lost.
Comprehensive treatment of arthrosis includes drugs that have anti-inflammatory and analgesic properties, and physiotherapy procedures that have an analgesic effect on the joints should also be carried out. If the treatment is carried out in a spa resort, then it consists in climatic conditions that favorably affect the joints, as well as in the use of mineral waters and mud.
The treatment of osteoarthritis is based on several basic principles:
Damaged joints must be spared from excessive stress. If possible, for the duration of treatment, it should be generally minimized.
Following the established orthopedic regimen.
Physiotherapy exercises.
Passing a course of physiotherapy, which includes magneto and electrotherapy, shock wave, and laser therapy.
Sanatorium treatment. For this, it is necessary once a year, on the recommendation of a doctor, to undergo a course of treatment at specialized resorts.
Saturation of the joint with oxygen, or the so-called intra-articular oxygen therapy.
Therapy with drugs.
Intraosseous blockades, as well as decompression of the metaepiphysis.
Rational approach to nutrition.
[Video] Dr. Evdokimenko – Treatment of arthrosis of the knee joint:









