Contents
What is gastrointestinal bleeding?
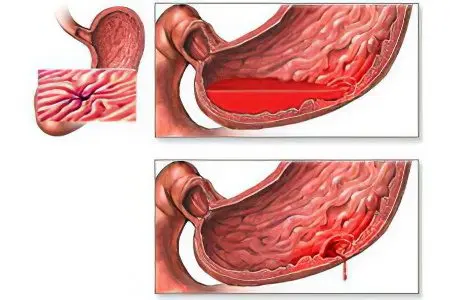
Gastrointestinal bleeding (ZHKK) is the outflow of blood from blood vessels damaged by the disease in the cavity of the organs of the gastrointestinal tract. Gastrointestinal bleeding is a common and serious complication of a wide range of pathologies of the gastrointestinal tract, posing a threat to the health and even life of the patient. The volume of blood loss can reach 3-4 liters, so this bleeding requires emergency medical care.
In gastroenterology, gastrointestinal bleeding is the 5th most common after appendicitis, pancreatitis, cholecystitis, and strangulated hernia.
The source of bleeding can be any part of the gastrointestinal tract. In this regard, bleeding from the upper gastrointestinal tract (from the esophagus, stomach, duodenum) and lower gastrointestinal tract (small and large intestines, rectum) are distinguished.
According to the etiological basis, ulcerative and non-ulcerative gastrointestinal tracts are distinguished, according to the nature of the bleeding itself – acute and chronic, according to the clinical picture – obvious and hidden, according to the duration – single and recurrent.
The risk group includes men of the age group of 45-60 years. 9% of people brought to the surgical departments by the ambulance service arrive there with gastrointestinal bleeding. The number of its possible causes (diseases and pathological conditions) exceeds 100.
Causes of stomach bleeding
All gastrointestinal bleeding is divided into four groups:
Bleeding in diseases and lesions of the gastrointestinal tract (peptic ulcer, diverticula, tumors, hernias, hemorrhoids, helminths, etc.);
Bleeding due to portal hypertension (hepatitis, cirrhosis of the liver, cicatricial strictures, etc.);
Bleeding in case of vascular damage (varicose veins of the esophagus, scleroderma, etc.);
Bleeding in blood diseases (aplastic anemia, hemophilia, leukemia, thrombocythemia, etc.).
Bleeding in diseases and lesions of the gastrointestinal tract
In the first group, ulcerative and non-ulcerative gastrointestinal tracts are distinguished. Ulcerative pathologies include:
Stomach ulcer;
Duodenal ulcer;
Chronic esophagitis (inflammation of the esophageal mucosa);
Gastroesophageal reflux disease of the esophagus (develops as a result of systematic spontaneous reflux of stomach contents into the esophagus);
Erosive hemorrhagic gastritis;
Nonspecific ulcerative colitis and Crohn’s disease (pathologies of the large intestine, similar in symptoms, but having a different etiology).
There are also the following causes leading to acute gastrointestinal ulcers:
Medications (long-term use of glucocorticosteroids, salicylates, NSAIDs, etc.);
Stress (mechanical injuries, burns, foreign bodies entering the gastrointestinal tract, emotional shock after injuries, operations, etc.);
Endocrine (Zollinger-Ellison syndrome (release of biologically active substance gastrin by an adenoma (tumor) of the pancreas) hypofunction of the parathyroid glands);
Postoperative (previously performed operations on the gastrointestinal tract).
Bleeding of a non-ulcer nature can be caused by:
Erosions of the gastric mucosa;
Mallory-Weiss syndrome (rupture of the mucous membrane at the level of the esophageal-gastric junction with recurrent vomiting);
Diverticula of the gastrointestinal tract (protrusion of the walls);
Diaphragmatic hernia;
bacterial colitis;
Hemorrhoids (inflammation and pathological expansion of the veins of the rectum, forming nodes);
anal fissures;
Benign tumors of the gastrointestinal tract (polyps, lipoma, neuroma, etc.);
Malignant tumors of the gastrointestinal tract (cancer, sarcoma);
Parasitic lesions of the intestine;
Infectious lesions of the intestine (dysentery, salmonellosis).
Bleeding due to portal hypertension
The cause of gastrointestinal bleeding of the second group can be:
chronic hepatitis;
Cirrhosis of the liver;
Thrombosis of the hepatic veins;
Thrombosis of the portal vein;
Compression of the portal vein and its branches with scar tissue or tumor formation.
Bleeding due to vascular injury

The third group includes gastrointestinal bleeding caused by damage to the walls of blood vessels. They are caused by the following diseases:
Atherosclerosis of vessels of internal organs;
Vascular aneurysms (expansion of the lumen of the vessel with simultaneous thinning of its walls);
Varicose veins of the esophagus or stomach (often resulting from impaired liver function);
Systemic lupus erythematosus (an immune disease that affects the connective tissue and capillaries;
Scleroderma (systemic disease causing sclerosis of small capillaries);
Hemorrhagic vasculitis (inflammation of the walls of blood vessels of internal organs);
Rendu-Osler disease (congenital vascular anomaly, accompanied by the formation of multiple telangiectasias);
Nodular periarteritis (damage to the arteries of the internal organs);
Thrombosis and embolism of the vessels of the mesentery of the intestine;
Cardiovascular pathologies (heart failure, septic endocarditis (damage to the heart valves), constrictive pericarditis (inflammation of the pericardial sac), hypertension).
Bleeding in blood diseases
The fourth group of gastrointestinal bleeding is associated with blood diseases such as:
Hemophilia and von Willebrand’s disease are genetically determined disorders of blood clotting);
Thrombocytopenia (deficiency of platelets – blood cells responsible for its clotting);
Acute and chronic leukemias;
Hemorrhagic diathesis (thrombasthenia, fibrinolytic purpura, etc. – a tendency to recurrent bleeding and hemorrhage);
Aplastic anemia (impaired function of the hematopoiesis of the bone marrow).
Consequently, gastrointestinal tract can occur both due to a violation of the integrity of the vessels (with their ruptures, thrombosis, sclerosis), and due to violations of hemostasis. Often both factors are combined.
With ulcers of the stomach and duodenum, bleeding begins as a result of melting of the vascular wall. This usually happens with the next exacerbation of a chronically occurring disease. But sometimes there are so-called silent ulcers that do not make themselves known until bleeding.
In infants often the cause of intestinal bleeding is volvulus. Bleeding with it is rather poor, the main symptoms are more pronounced: an acute attack of abdominal pain, constipation, and non-excretion of flatus. In children under the age of three, such bleeding is more often caused by anomalies in the development of the intestine, the presence of neoplasms, and diaphragmatic hernia. Older children are more likely to have colon polyps, in which case some blood is shed at the end of a bowel movement.
Signs and symptoms of stomach bleeding

Common symptoms of gastrointestinal bleeding are as follows:
Weakness;
Nausea, vomiting with blood;
Dizziness;
Pale skin, blue lips and fingertips;
changed chair;
Cold sweat;
Weak, rapid pulse;
Lowering blood pressure.
The severity of these symptoms can vary widely, from mild malaise and dizziness to deep fainting and coma, depending on the rate and volume of blood loss. With slow, weak bleeding, their manifestations are insignificant, there is a slight tachycardia at normal pressure, since partial compensation for blood loss has time to occur.
GI symptoms are usually accompanied by signs of the underlying disease. In this case, pain in different parts of the gastrointestinal tract, ascites, signs of intoxication can be observed.
In acute blood loss, a short-term fainting is possible due to a sharp drop in pressure. Symptoms of acute bleeding:
Weakness, drowsiness, severe dizziness;
Darkening and “flies” in the eyes;
Noise in ears;
Shortness of breath, severe tachycardia;
increased sweating;
Cold feet and hands;
Weak pulse and low blood pressure.
Symptoms of chronic bleeding are similar to signs of anemia:
Deterioration of the general condition, high fatigue, decreased performance;
Pale skin and mucous membranes;
Dizziness;
The presence of glossitis, stomatitis, etc.
The most characteristic symptom of gastrointestinal bleeding is blood in the vomit and stool. Blood in the vomit may be present unchanged (with bleeding from the esophagus in case of varicose veins and erosions) or in an altered form (with stomach and duodenal ulcers, as well as Mallory-Weiss syndrome). In the latter case, the vomit has the color of “coffee grounds”, due to the mixing and interaction of blood with hydrochloric acid from the contents of gastric juice. The blood in the vomit is bright red in profuse (massive) bleeding. If hematemesis occurs again after 12-1 hours, most likely, the bleeding continues, if after 2-4 hours, this is more indicative of re-bleeding. With bleeding from the lower gastrointestinal tract, vomiting is not observed.
In the stool, blood is present in unchanged form with a single blood loss exceeding 100 ml (during the outflow of blood from the lower part of the gastrointestinal tract and with a stomach ulcer). In an altered form, blood is present in the stool during prolonged bleeding. In this case, 4-10 hours after the bleeding began, a tarry stool of a dark, almost black color (melena) appears. If during the day less than 100 ml of blood enters the gastrointestinal tract, visual changes in the stool are not noticeable.
If the source of bleeding is in the stomach or small intestine, the blood, as a rule, is evenly mixed with feces; when it flows out of the rectum, the blood looks like separate clots on top of the feces. Isolation of scarlet blood indicates the presence of chronic hemorrhoids or anal fissure.
It should be taken into account that the stool may have a dark color when eating blueberries, chokeberries, beets, buckwheat porridge, taking activated charcoal, iron and bismuth preparations. Also, the cause of tarry stools can be the ingestion of blood during pulmonary or nosebleeds.
For gastric and duodenal ulcers, a decrease in ulcer pain during bleeding is characteristic. With heavy bleeding, the stool becomes black (melena) and liquid. During bleeding, there is no tension in the abdominal muscles and no other signs of peritoneal irritation appear.
In gastric cancer, along with the typical symptoms of this disease (pain, weight loss, lack of appetite, change in taste preferences), recurrent, weak bleeding, tarry stools are observed.
With Mallory-Weiss syndrome (rupture of the mucosa), profuse vomiting occurs with an admixture of scarlet unaltered blood. With varicose veins of the esophagus, bleeding and its clinical symptoms develop acutely.
With hemorrhoids and anal fissures, scarlet blood can be released at the time of defecation or after it, as well as during physical exertion, it does not mix with feces. Bleeding is accompanied by anal itching, burning, spasms of the anal sphincter.
With cancer of the rectum and colon, bleeding is prolonged, not intense, dark blood is mixed with feces, mucus impurities are possible.
In ulcerative colitis and Crohn’s disease, watery stools mixed with blood, mucus and pus are observed. With colitis, false urges to defecate are possible. In Crohn’s disease, bleeding is mostly mild, but the risk of heavy bleeding is always high.
Profuse gastrointestinal bleeding has four degrees of severity:
Relatively satisfactory condition, the patient is conscious, the pressure is normal or slightly lower (not lower than 100 mm Hg), the pulse is slightly increased, as the blood begins to thicken, the level of hemoglobin and red blood cells is normal.
Condition is moderate, marked pallor, acceleration of the heart rate, cold sweat, pressure drops to 80 mm Hg. Art., hemoglobin – up to 50% of the norm, blood clotting decreases.
Severe condition, there is lethargy, swelling of the face, pressure below 80 mm Hg. Art., pulse above 100 beats. per minute, hemoglobin – 25% of the norm.
Coma and the need for resuscitation.
First aid for gastrointestinal bleeding

Any suspicion of GIB is an urgent reason to call an ambulance and deliver a person to a medical facility on a stretcher.
Prior to the arrival of doctors, the following first aid measures should be taken:
Lay the person on their back with their legs slightly raised and ensure complete rest.
Exclude food intake and do not give to drink – this stimulates the activity of the gastrointestinal tract and, as a result, bleeding.
Put dry ice or any other cold object on the area of u15bu20bthe alleged bleeding – the cold narrows the blood vessels. It is better to apply ice for 2-3 minutes with XNUMX-XNUMX minute breaks to prevent frostbite. Additionally, you can swallow small pieces of ice, but with gastric bleeding it is better not to risk it.
You can give to take 1-2 teaspoons of a 10% solution of calcium chloride or 2-3 crushed Dicinon tablets.
It is forbidden to put an enema and wash the stomach. When fainting, you can try to bring to life with the help of ammonia. When unconscious, monitor your pulse and breathing.
Complications of gastrointestinal bleeding
Gastrointestinal bleeding can lead to such dangerous complications as:
hemorrhagic shock (as a consequence of profuse blood loss);
acute anemia;
acute renal insufficiency;
multiple organ failure (stress reaction of the body, which consists in the combined failure of several functional systems).
Untimely hospitalization and attempts at self-treatment can lead to death.
Diagnosis of gastric bleeding
Gastrointestinal bleeding must be distinguished from pulmonary nasopharyngeal bleeding, in which blood can be swallowed and end up in the gastrointestinal tract. Similarly, when vomiting, blood can enter the respiratory tract.
Differences between bloody vomiting and hemoptysis:
Blood leaves with vomiting, and with hemoptysis – during coughing;
With vomiting, the blood has an alkaline reaction and has a bright red color, with hemoptysis – an acidic reaction and has a maroon color;
With hemoptysis, the blood may foam, while vomiting does not;
Vomiting is profuse and short-lived, hemoptysis may last several hours or days;
Vomiting is accompanied by dark stools; this is not present with hemoptysis.
Profuse GCC must be differentiated from myocardial infarction. With bleeding, the decisive sign is the presence of nausea and vomiting, with a heart attack – retrosternal pain. In women of reproductive age, intra-abdominal bleeding due to ectopic pregnancy should be excluded.
The diagnosis of GI is based on:
History of life and anamnesis of the underlying disease;
Clinical and rectal examination;
General blood test and coagulogram;
Analysis of feces for occult blood;
Instrumental studies, among which the main role belongs to endoscopic examination.
When analyzing the anamnesis, information is obtained about previous and existing diseases, the use of certain medications (Aspirin, NSAIDs, corticosteroids) that could provoke bleeding, the presence / absence of alcohol intoxication (which is a common cause of Mallory-Weiss syndrome), and the possible influence of harmful working conditions.
Clinical examination
Clinical examination includes examination of the skin (staining, presence of hematomas and telangiectasias), digital examination of the rectum, assessment of the nature of vomit and feces. The condition of the lymph nodes, the size of the liver and spleen, the presence of ascites, tumor neoplasms and postoperative scars on the abdominal wall are analyzed. Palpation of the abdomen is carried out very carefully so that bleeding does not increase. With bleeding of non-ulcer origin, there is no pain reaction to palpation of the abdomen. Enlarged lymph nodes are a sign of a malignant tumor or a systemic blood disease.
Yellowness of the skin in combination with ascites may indicate a pathology of the biliary system and allows us to consider varicose veins of the esophagus as a possible source of bleeding. Hematomas, spider veins and other types of skin hemorrhages indicate the possibility of hemorrhagic diathesis.
On examination, it is impossible to determine the cause of bleeding, but you can roughly determine the degree of blood loss and the severity of the condition. Lethargy, dizziness, “flies before the eyes”, acute vascular insufficiency indicate cerebral hypoxia.
It is important to study the rectum with a finger, which helps to analyze the state of not only the intestine itself, but also nearby organs. Pain during examination, the presence of polyps or bleeding hemorrhoids allow us to consider these formations as the most likely sources of bleeding. In this case, after a manual examination, instrumental (rectoscopy) is performed.
Laboratory methods

Laboratory methods include:
Complete blood count (analysis of hemoglobin and other major blood cells, calculation of leukocyte formula, ESR). In the first hours of bleeding, the composition of the blood changes slightly, only moderate leukocytosis is observed, sometimes a small increase in platelets and ESR. On the second day, the blood thins, hemoglobin and red blood cells fall (even if the bleeding has already stopped).
Coagulogram (determining the term of blood clotting, etc.). After acute profuse bleeding, the activity of blood clotting increases markedly.
Biochemical blood test (urea, creatinine, liver tests). Usually, urea rises against the background of normal creatinine levels. All blood tests are of diagnostic value only when viewed over time.
Instrumental diagnostic methods:
Instrumental diagnostic methods include:
X-ray examination determines ulcers, diverticula, other neoplasms, is not effective for detecting gastritis, erosion, portal hypertension, and bleeding from the intestine.
Endoscopy surpasses X-ray methods in accuracy and allows to detect superficial lesions of the mucous membranes of organs. Types of endoscopy are fibrogastroduodenoscopy, rectoscopy, sigmoidoscopy, colonoscopy, which in 95% of cases allow you to determine the source of bleeding.
Radioisotope research confirm the presence of bleeding, but are ineffective in determining its exact localization.
Spiral contrast computed tomography allows you to determine the source of bleeding when it is in the small and large intestine.
Treatment of gastrointestinal bleeding
Patients with acute GI bleeding are admitted to the intensive care unit, where the following measures are taken in the first place:
catheterization of the subclavian or peripheral veins in order to quickly replenish the volume of circulating blood and determine the central venous pressure;
probing and washing the stomach with cold water to remove accumulated blood and clots;
bladder catheterization to control diuresis;
oxygen therapy;
cleansing enema to remove blood that has flowed into the intestines.
Conservative treatment
Conservative treatment is indicated for:
hemorrhagic diathesis, vasculitis and other diseases caused by violations of the mechanisms of hemostasis, since in this case the bleeding will become more intense during surgery;
severe cardiovascular pathologies (heart disease, heart failure);
severe underlying disease (leukemia, inoperable tumors, etc.).
Conservative therapy includes three groups of therapeutic measures aimed at:
hemostasis system;
Source of bleeding;
Restoration of the normal volume of circulating blood (infusion therapy).
To influence the hemostasis system, Etamzilat, Thrombin, Aminocaproic acid, Vikasol are used. The basic drug is Octreotide, which lowers pressure in the portal vein, reduces the secretion of hydrochloric acid, and increases platelet activity. If oral administration of drugs is possible, Omeprazole, Gastrocepin are prescribed, as well as Vasopressin, Somatostatin, which reduce the blood supply to the mucous membranes.
With ulcerative bleeding, Famotidine, Pantoprazole are administered intravenously. The introduction of liquid Fibrinogen or Dicinon during an endoscopic procedure near the ulcer can stop bleeding.
Infusion therapy begins with the infusion of rheological solutions that stimulate microcirculation. With blood loss of the 1st degree, Reopoliglyukin, Albumin, Hemodez are administered intravenously with the addition of glucose and salt solutions. With blood loss of the 2nd degree, plasma-substituting solutions and donor blood of the same group and Rh factor are infused at the rate of 35-40 ml per 1 kg of body weight. The ratio of plasma solutions and blood is 2:1.
With blood loss of the 3rd degree, the proportions of infused solutions and blood should be 1:1 or 1:2. The volume of infusions must be clearly calculated, since excessive administration of drugs can provoke a recurrence of bleeding. The total dose of infusion solutions should exceed the amount of blood lost by about 200-250%.
With bleeding of 1 degree of severity, there is no need for surgical intervention.
With bleeding of the 2nd degree of severity, conservative treatment is carried out, and if it was possible to stop it, the need for surgery disappears.
Surgery
With grade 3 bleeding, profuse and recurrent, surgical treatment is often the only possible way to save the patient. An emergency operation is necessary in case of perforation of the ulcer and the inability to stop the bleeding by conservative (endoscopic and other) methods. The operation must be carried out in the early stages of bleeding, as with late interventions, the prognosis deteriorates sharply.
With bleeding ulcers of the stomach and duodenum, a stem vagotomy is performed with partial resection of the stomach, gastrotomy with excision of the ulcer or stitching of damaged vessels. The possibility of death after surgery is 12-5%. In Mallory-Weiss syndrome, tamponade is applied using a Blackmore probe. If it is ineffective, the mucous membrane is sutured at the site of the rupture.
Diet for stomach bleeding

Eating is allowed only one or two days after the cessation of severe gastrointestinal bleeding. Dishes should be chilled and have a liquid or semi-liquid appearance: mashed soups, mashed potatoes, cereals, yogurts, jelly, jelly.
As the condition improves, the diet expands: meat soufflé, soft-boiled eggs, scrambled eggs, boiled vegetables, steam fish, baked apples are gradually added to it. Frozen cream, milk, butter are recommended.
When the patient’s condition stabilizes (about 5-6 days), food is taken every two hours. The daily volume of food should not exceed 400 ml.
To reduce hemorrhagic syndrome, you should eat foods rich in vitamins C, P (fruit and vegetable juices, rosehip broth) and K (butter, cream, sour cream). Animal fats increase blood clotting and promote faster clot formation in peptic ulcers.









