Contents
What is reactive arthritis?
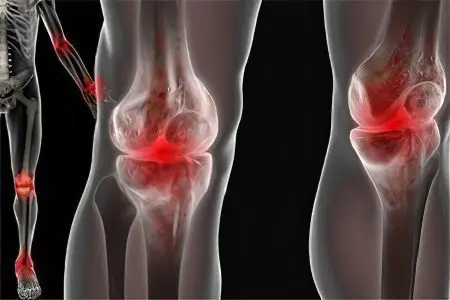
Reactive arthritis – This is a serious disease of the joints, which has its own characteristic features.
This form of arthritis is accompanied by one or more of the following symptoms:
Inflammatory processes in the organs of the gastrointestinal tract.
Conjunctivitis (inflammation of the eyes).
Inflammatory processes in the genitourinary system.
Inflammation of the joints.
According to available statistics, the data of which are published in specialized medical publications and the media, reactive arthritis is most often diagnosed in patients whose age ranges from 30 to 40 years. In men, most cases of the disease were detected, which provoked a genitourinary infection. Representatives of the female and male half of the population are equally often diagnosed with reactive arthritis, which develops against the background of the progression of an intestinal infection (dysentery).
According to many experts, reactive arthritis is a rheumatic disease that, in the active stage of its development, can affect the vital organs and systems of the human body.
Most often, problems occur in the following organs:
in the lungs;
in the kidneys;
in the heart;
in the soft tissues of the organs of vision;
on the skin (in the form of a rash, sores or urticaria);
on the oral mucosa, etc.
In recent years, it is the reactive form of arthritis that is most often diagnosed in the population of different countries of the world, causing severe damage to the musculoskeletal system in people, regardless of age and gender. Many rheumatologists believe that if reactive arthritis was not triggered by an intestinal or urogenital infection, then it should be classified as Reiter’s disease. This is due to the fact that only in 4% of cases with this form of arthritis, infections of the genitourinary system were detected.
Reactive Arthritis Symptoms

At the initial stage of development, reactive arthritis in most patients manifests itself in an acute form.
According to the results of numerous studies, it was found that the first symptoms of this disease appear 2 weeks after the infection of the patient:
The temperature rises in the area of the affected joints. To determine the heat in the joint, it is enough to put your palm on the injury site. To relieve the heat, it is recommended to use compresses.
Joints swell (ankle and knee, as well as elbow and wrist joints, joints of the hands and feet). Sometimes the swelling spreads rapidly beyond the contours of the joints.
Pain develops in the joints. There are pain sensations, mainly when walking, or performing other movements with the affected lower or upper limb. Many patients experience dull, twisting, or aching pain with any physical movement that subsides somewhat at night. They also experience discomfort during palpation of the area affected by the disease of the joint.
There is stiffness of movements caused by a violation of the outflow of joint fluid. Sick people can not actively move, do physical exercises.
An articular syndrome appears, which is accompanied by pain, asymmetric oligoarthritis, joint damage, swelling, etc.
Infections are detected in the genitourinary system, nasopharynx, intestines (accompanied by characteristic symptoms). Urogenital infections accompany such diseases of the genitourinary system as urethritis and cervicitis, and complications that develop against their background.
There is an expansion of the joint space and edema (periarticular) of the soft tissues (easily determined by radiography).
Inflamed eyes, skin (conjunctivitis, irritation of the mucosa, weakening of visual activity, urticaria, psoriasiform rashes, stomatitis, etc.).
In the initial stage of the development of reactive arthritis, patients show signs of sacroiliitis (damage to the spine), kidney disease, heart disease (tachycardia), and nervous system disorders.
Fatigue, loss of working capacity.
General malaise, sudden weight loss.
Feverish conditions, often accompanied by an increase in temperature, or chills, etc.
Causes of Reactive Arthritis
According to the results of numerous studies conducted by specialists from around the world, it was found that reactive arthritis in most cases develops against the background of poor heredity. Modern medicine is able to detect this disease at the genetic level. This is due to special laboratory studies that use reagents that determine the genetic markers of HLA-B27. Despite hereditary predisposition, reactive arthritis will only appear in patients when they are infected with the disease.
The causes of reactive arthritis include the following provoking factors:
various bacteria (Salmonella, Yersinia, Shigella, Campylobacter);
infectious diseases (dysentery);
abnormalities in the patient’s immune system;
genetic predisposition to this disease (reactive arthritis is most often detected in carriers of the HLA-B27 antigen);
infection of the patient with harmful microorganisms penetrating the human genitourinary system (for example, chlamydia Chlamydia trachomatis, Ureaplasma urealyticum), etc.
Diagnosis of reactive arthritis

If characteristic symptoms or any discomfort in the area of the joints are detected, the patient should contact a narrow-profile specialist – a rheumatologist.
At the appointment, the doctor must correctly collect the history of this disease, and then assign the patient a complex of laboratory tests and hardware diagnostics:
clinical and biochemical blood tests;
general urine analysis;
other blood tests, through which the following indicators are determined: antibodies, antigen, sialic acids, etc.;
smears from the cervical canal and urethra;
enzyme immunoassay;
sowing feces to identify pathogenic microflora;
PCR analysis;
sigmoidoscopy;
radiography (of the spinal column, joints of the lower and upper extremities);
fibrocolonoscopy;
magnetic resonance or computed tomography, etc.
Diagnosis of reactive arthritis is carried out on the basis of data from the initial examination, during which the specialist identified the main signs of this disease, and the results of a laboratory and hardware examination of the patient. Thanks to timely radiography, the doctor can detect any, even minor, changes in the musculoskeletal system. Sometimes hardware diagnostics can detect calcifications, which are located on the bone tissues, in the area of which inflammatory processes occurred.
If a patient who has been diagnosed with reactive arthritis has inflammation of the eyes, then the attending physician refers him for a consultation with an ophthalmologist. A narrow-profile specialist will not only determine visual acuity, but also identify the degree of inflammation, after which he will prescribe drug therapy.
Treatment of reactive arthritis
After a comprehensive diagnosis of reactive arthritis, the specialist chooses the method by which this disease will be treated. The method of therapy will directly depend on the location of the disease and on the stage of its development.
In most cases, this category of patients is assigned:
Non-steroidal drugs with anti-inflammatory action. Against the background of their regular intake, patients may experience various side effects: ulcers appear, gastrointestinal disorders develop, internal bleeding begins.
In the treatment of reactive arthritis, patients are prescribed corticosteroids. This group of drugs, including prednisolone, can significantly reduce the inflammatory process in the joints and tendons of the upper and lower extremities. They can be taken in any convenient way: in the form of ointments; in tablet form orally; in the form of injections (introduced into the affected joint).
In the event that a patient has a reactive form of arthritis provoked by sexually transmitted or viral infections, he is prescribed a course of antibiotics.
In parallel, the patient should take probiotics, the functions of which are to mitigate the effects of antibiotics on the human gastrointestinal tract.
Patients who have been diagnosed with a persistent form of reactive arthritis are prescribed sulfazilin. This medicine may come with various side effects such as bone marrow suppression, skin rashes. After a course of sulfazilin, patients should undergo a laboratory examination and take blood tests.
In inflammatory processes in the eyes of patients, special drops are prescribed. A severe form of inflammation will require more serious treatment, which includes injections of cortisone.
With an inflammatory process in the area of uXNUMXbuXNUMXbthe male or female genitalia, the attending physician prescribes a course of therapy with creams, which include cortisone.
In reactive arthritis caused by intestinal or urogenital infections, patients are prescribed antibiotics specific to the identified groups of bacteria.
If an inflammatory effusion has been detected in a patient, then specialists carry out a set of measures to evacuate him from the damaged joint cavity of the upper or lower limb. In parallel, this category of patients is prescribed ointments, creams, gels, which contain dimexide, which has an anti-inflammatory effect.
Patients diagnosed with reactive arthritis are recommended various physiotherapy procedures, such as cryotherapy, phonophoresis, sinusoidal modulating currents, etc. A great benefit in the treatment of this disease comes from a course of physical therapy, during which patients perform specially designed exercises under the supervision of an experienced instructor.
After the removal of the inflammatory process in the area of damaged joints, patients are prescribed therapeutic baths. During such water procedures, salts from the Dead Sea, as well as hydrogen sulfide and hydrogen sulfide salts are usually used. In parallel with therapeutic baths, you can take a course of mud therapy.
Regardless of what therapy has been used in the treatment of reactive arthritis, patients are advised to take tests at regular intervals that can show the presence of infection. If any bacteria that can provoke the re-development of reactive arthritis are detected, patients are prescribed a course of therapy that includes a new group of antibiotics (when choosing the most effective drugs, patients are advised to take a special analysis).
Prognosis of the disease

For patients who have undergone complex treatment for reactive arthritis, there is the following prognosis for later life:
in 20% of cases, the signs of the disease disappear within 6 months;
after properly selected treatment, there is no recurrence of the disease;
in 25% of cases, reactive arthritis becomes chronic, progressing only in the acute phase;
in 50% of cases, the disease after a certain period of time begins to progress with renewed vigor;
only in 5% of cases, a severe form of reactive arthritis leads to deformation of the spine and joints.
Prevention of reactive arthritis
In order to prevent reactive arthritis, experts recommend a set of measures:
avoid casual sexual intercourse, during which you can become infected with urogenital infections;
observe personal hygiene;
lead a healthy lifestyle;
eat healthy foods;
undergo a medical examination in a timely manner, etc.









