Contents
What is plague?
Plague is an extremely dangerous, acute zoonotic transmissible infection that causes severe intoxication, as well as serous-hemorrhagic inflammation in the lungs, lymph nodes and other organs, and it is often accompanied by the development of sepsis.
Brief historical information
In the entire history of mankind, there has never been such a ruthless infectious disease as the plague. It devastated the cities, causing a record death rate of the population. Information has reached our time that in ancient times plague epidemics claimed a huge number of human lives. As a rule, epidemics began after contacts of people with infected animals. Often the spread of this disease turned into a pandemic, three such cases are known.
The first pandemic, called the Justinian Plague, was recorded in Egypt and the Eastern Roman Empire in the period from 527 to 565. The second was called the “great” and “black” death, for 5 years, starting from 1345, it raged in the countries of the Mediterranean, Western Europe and in the Crimea, taking with it about 60 million human lives. The third pandemic began in Hong Kong in 1895 and later spread to India, where more than 12 million people died.
During the last pandemic, important discoveries were made, thanks to which it became possible to carry out the prevention of the disease, guided by data on the identified plague pathogen. It has also been proven that rats contribute to the spread of infection. In 1878, Professor G. N. Minkh discovered the causative agent of the plague; also in 1894, scientists S. Kitazato and A. Yersen worked on this issue.
There were plague epidemics in Russia as well – starting from the XNUMXth century, this terrible disease periodically declared itself. Many Russian scientists have made a great contribution to the study of this disease. Such scientists as I. I. Mechnikov, D. K. Zabolotny, N. F. Gamaleya, and N. N. Klodnitsky prevented the spread of the epidemic and treated the sick. And in the XNUMXth century, G. P. Rudnev, N. N. Zhukov-Verezhnikov and E. I. Korobkova developed the principles of diagnosis and pathogenesis of the plague, and a vaccine against this infection was created and ways to treat the disease were determined.
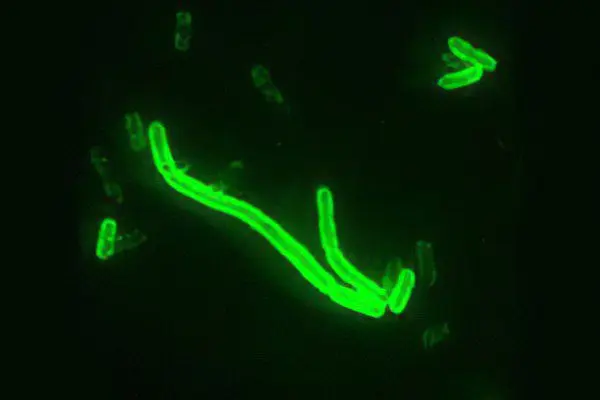
What causes plague?
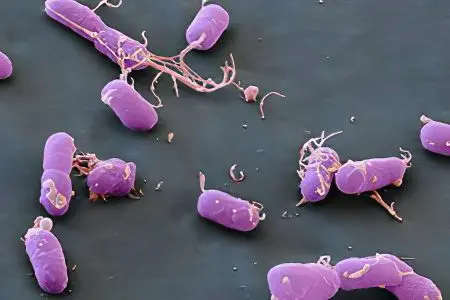
The causative agent of infection is a non-motile gram-negative facultative anaerobic bacterium Y. pestis, which belongs to the genus Yersinia and the family Enterobacteriaceae. In its biochemical and morphological characteristics, the plague bacillus resembles the causative agents of diseases such as pseudotuberculosis, pasteurellosis, yersiniosis and tularemia – people and rodents are susceptible to them. The causative agent is characterized by polymorphism, it has the appearance of an ovoid rod, which is bipolar colored. There are several subspecies of this pathogen, which differ in virulence.
The growth of the pathogen occurs in a nutrient medium; to stimulate growth, it needs sodium sulfite or hemolyzed blood. More than 30 antigens, as well as exo- and endotoxins, were found in the composition. The absorption of bacteria by polymorphonuclear leukocytes is prevented by capsules, and V- and W-antigens protect from lysis in the cytoplasm of phagocytes, which is why they multiply inside the cells.
The causative agent of the plague is able to persist not only in infected excreta, but also various objects of the external environment contain it. For example, in the pus of a bubo, it can persist for 30 days, and in the corpses of rodents, camels and people – about two months. The sensitivity of the pathogen to sunlight, oxygen, high temperatures, acidic reactions, as well as some chemicals and disinfectants has been noted. A solution of sublimate (1:1000) is able to destroy the pathogen in 2 minutes. But the pathogen tolerates low temperatures and freezing well.
Epidemiology
The main source of plague, as well as its reservoir, are wild rodents, of which there are about 300 species, and they are ubiquitous. But not all animals are capable of retaining the pathogen. In each natural focus, there are main species that store and carry the infection. The main natural sources are ground squirrels, marmots, voles, gerbils, pikas and others. For anthropurgic foci of plague – cities, ports, the main threat is synanthropic rats. Among them, one can distinguish a gray rat, which is also called pasyuk. She usually lives in the sewer system of large cities. And also black – Egyptian or Alexandrian rat, living in houses or on ships.
Dogs are resistant to the distemper pathogen, but fleas can become infected from them. There are more and more cases of infection in cats, which can transmit the infection to humans. From a camel, a person can also take over the infection. Plague infection is preserved by transmitting the pathogen of infected animals to healthy ones, in this a special role is played by fleas that parasitize rodents.
If an acute form of the disease develops in rodents, then the animals quickly die, and the spread of infection (epizooty) stops. But some rodents, for example, marmots, ground squirrels, tarbagans, falling into hibernation, carry the disease in a latent form, and in the spring they become sources of plague, which is why a natural focus of infection appears in their habitat.
Infected people also become sources of plague. For example, if a person has a disease such as pneumonic plague, and also if contact with bubo pus occurs, or if fleas are infected from a patient with plague septicemia. Often the cause of the spread of infection are the corpses of plague patients. Of all these cases, people infected with pneumonic plague are considered especially dangerous.
There are quite a few ways of transmitting the infection, but the main one is transmissible, but with a pulmonary form of the disease, infection can occur by airborne droplets. Carriers are not only fleas (there are about 100 species), but also ticks that support the epizootic process in nature, transmitting the infection to rodents, cats, dogs and camels, and they, in turn, transfer these parasites to human habitation.
The infection is transmitted to a person from fleas not so much through a bite, but because after that feces or regurgitated masses of an insect are rubbed into the skin. Bacteria that produce coagulase multiply in the intestines of an infected flea. This substance forms a kind of plug or plague block, and it blocks the flow of blood into her body. As a result, the parasite, trying to get enough, regurgitates infected masses onto the skin at the site of the bite. These insects, experiencing a feeling of hunger, try to get enough through animals. Fleas usually remain contagious for about 7 weeks, but there is evidence that some individuals can be carriers for up to a year.
You can also get infected by contact, for example, through the mucous membrane or damage to the skin. This can happen when cutting and processing the carcasses of infected animals (hares, foxes, saigas and others), as well as when eating this meat.
People are very susceptible to infection, regardless of the mode of infection and the age group to which the person belongs. If a person has had the plague, he has some immunity to this disease, but the possibility of re-infection is not excluded. Moreover, being infected with plague a second time is not a rare case, and the disease takes place in an equally severe form.
The main epidemiological signs of plague
Plague foci in nature can occupy about 7% of the land, and have been reported on almost all continents (the only exceptions are Australia and Antarctica). Every year, several hundred people around the world are infected with the plague. On the territory of the CIS, 43 natural foci were identified, the area of which is at least 216 million hectares. The outbreaks are located on the plains – desert, steppe, and in highlands.
Natural foci are divided into two types: “wild” and rat plague. Under natural conditions, the plague has the form of an epizootic of rodents and lagomorphs. The rodents sleeping in winter carry the disease in the warm season (spring), and animals that do not hibernate contribute to the formation of two seasonal peaks of the plague, which occur at the time of their active reproduction. As a rule, men are more likely to become infected with plague – this is due to the fact that they are forced to stay in the natural focus of the plague more often (activities associated with hunting, animal husbandry). In the conditions of the city, the role of carriers is assumed by rats – gray and black.
If we compare the epidemiology of two types of plague – bubonic and pneumonic, we can note significant differences. First of all, bubonic plague develops quite slowly, and the pneumonic form can spread very widely in the shortest possible time – this is due to the easy transmission of bacteria. People suffering from bubonic plague are almost non-contagious and not contagious. There are no pathogens in their secretions, and there are quite a few of them in the pus of buboes.
If the disease has passed into a septic form or bubonic plague has complications with secondary pneumonia, which allows the pathogen to be transmitted by airborne droplets, epidemics of primary type pneumonic plague begin, which is characterized by a high degree of contagiousness. Most often, pneumonic plague appears after bubonic plague, then spreads along with it and very quickly passes into the leading epidemiological and clinical form.
There is an opinion that the causative agent of infection is able to stay in the soil, being in an uncultivated state for a long time. At the same time, rodents that dig holes in infected soils receive a primary infection. Scientists confirm this hypothesis by experimental studies, as well as by the search for the plague pathogen among rodents in inter-epizootic periods, the ineffectiveness of which allows us to draw some conclusions.
Plague symptoms

It is known that the incubation period of the plague is from 3 to 6 days, but in an epidemic or septic form it can be reduced to 1 day. The maximum incubation period that has been recorded is 9 days.
The disease begins acutely, accompanied by a rapid increase in body temperature, severe chills and signs of intoxication. Patients often complain of pain in the muscles and joints, pain in the sacrum and in the head. A person vomits (sometimes with blood), is tormented by thirst. In the first hours of the disease, psychomotor agitation is observed. The patient becomes restless and too active, there is a desire to escape (this is where the saying “runs like crazy” takes its roots), then hallucinations and delirium appear. A person can no longer speak clearly and walk straight. Sometimes, on the contrary, they notice apathy and lethargy, and because of the weakness of the patient, he is not able to get out of bed.
Of the external signs, puffiness of the face, hyperemia, and injection of the sclera can be noted. The facial expression takes on a suffering look, it bears the mark of horror, or, as they say, the “mask of the plague”. In severe cases, a hemorrhagic rash appears on the skin. The tongue increases in size, covered with a white coating resembling chalk. Cardiac arrhythmia, tachycardia are also noted, blood pressure gradually decreases. Even local forms of the disease are characterized by the development of anuria, oliguria, tachypnea. These symptoms are more pronounced at the initial stage of the disease, but accompany all forms of plague.
In 1970, G.P. Rudnev proposed the following clinical classification of plague:
local forms (bubonic, skin and skin-bubonic);
generalized (primary and secondary septic);
externally disseminated (primary and secondary pulmonary, as well as intestinal).
Every form
This form of the disease is characterized by the appearance of a carbuncle in the place where the pathogen has invaded. First, a pustule forms on the skin (the appearance is accompanied by a sharp pain) with dark red contents. It is located on the subcutaneous edematous tissue, around it is a zone of hyperemia and infiltration. If the pustule is opened, an ulcer with a yellowish bottom appears in its place. Then this bottom is covered with a black scab, which is rejected, leaving behind scars.
bubonic form
This is the most common form of the disease. Bubonic plague infects the lymph nodes that are closest to the place of introduction of the pathogen. Usually these are inguinal nodes, sometimes – axillary, and less often – cervical. Most often buboes are single, but can be multiple. Pain occurs at the site of the next formed bubo, this is accompanied by intoxication.
It is possible to palpate the lymph nodes 1-2 days after their appearance, the hard consistency gradually changes to a softer one. The nodes are combined into an inactive conglomerate, which can fluctuate during palpation due to the presence of periadenitis in it. The disease develops for about 7 days, followed by a period of convalescence. Enlarged nodes can resolve, ulcerate or sclerosis, this is facilitated by necrosis and serous-hemorrhagic inflammation.
Skin-bubonic form
This form is a change in the lymph nodes and skin lesions. Local forms of the disease can turn into secondary pneumonia and secondary plague sepsis. The clinical characteristics of these forms do not differ from the primary forms of these same diseases.
The primary septic form appears with a short (1-2 days) incubation period and is accompanied by the rapid onset of intoxication, as well as hemorrhagic manifestations – gastrointestinal or renal bleeding, hemorrhages in the mucous membranes and skin. In the shortest possible time, an infectious-toxic shock develops. If the disease is not treated, then death is inevitable.
The primary pulmonary form appears after aerogenic infection. It has a short incubation period – it can be several hours, a maximum of two days. The disease develops acutely, first there is an intoxication syndrome. On the second or third day, there is a cough and pain in the chest, shortness of breath. When coughing, vitreous (at first), and then liquid, foamy sputum with blood is released.
The obtained physical data of the lungs are extremely scarce, signs of lobar or focal pneumonia are visible on the radiograph. Cardiovascular insufficiency increases, which is expressed in tachycardia and a gradual decrease in blood pressure, cyanosis develops. At the terminal stage, patients enter a soporous state, which is accompanied by shortness of breath, hemorrhagic manifestations (extensive hemorrhages), after which the person falls into a coma.
In the intestinal form, patients experience severe intoxication, and at the same time severe pain in the abdomen, constant vomiting and diarrhea, accompanied by tenesmus. Mucous and bloody discharges are visible in the stool. Other forms of plague are also characterized by similar manifestations (probably due to enteric infection), so the question of the existence of an intestinal form of this disease as an independent one remains controversial.
Plague diagnosis

Differential diagnostics
The various forms of plague – bubonic, skin, and skin-bubonic must be distinguished from diseases such as tularemia, lymphadenopathy, and from carbuncles. And the septic and pulmonary forms can have symptoms reminiscent of lung disease, sepsis, and meningococcal etiology.
All forms of plague are characterized by severe intoxication, the progressive signs of which appear at the very beginning of the disease. A person’s temperature rises, chills appear, he vomits, he is tormented by thirst. Psychomotor agitation, anxiety, hallucinations and delirium are also alarming. On examination, slurred speech, an unsteady gait are revealed, the face becomes puffy, an expression of suffering and horror appears on it, the tongue is white. Develops cardiovascular insufficiency, oliguria, tachypnea.
The skin and bubonic forms of the plague can be identified by sharp pain in the affected areas, it is easy to determine the stages of carbuncle development (first a pustule, then an ulcer, then a black scab and a scar), periadenitis is observed during the formation of a bubo.
Pulmonary and septic forms are accompanied by an extremely rapid development of intoxication, as well as manifestations of hemorrhagic syndrome and infectious-toxic shock. Damage to the lungs is accompanied by a sharp pain in the chest and a violent cough with vitreous, and after frothy sputum with blood. Physical data often do not correspond to the patient’s noticeable serious condition.
Laboratory diagnosis
This type of diagnosis is based on the use of biological and microbiological, immunoserological and genetic methods. The hemogram shows leukocytosis and neutrophilia with a shift to the left, as well as an increase in ESR. The causative agent is isolated in sensitive specialized laboratories designed specifically to work with pathogens of the most dangerous infections. Research is underway to confirm clinically apparent cases of plague, and examine people who are in the focus of infection, and their body temperature is above normal. Material taken from patients with plague or who died from this disease is subjected to bacteriological analysis. Punctates are taken from carbuncles and buboes, ulcers, sputum, mucus and blood are also examined. They conduct experiments with laboratory animals, which, after being infected with plague, can live for about 7 days.
As for serological methods, RNAG, RNGA, RNAT, RTPGA, ELISA are used. If PCR gives a positive result, then 6 hours after setting, we can talk about the presence of the DNA of the plague microbe and confirm the preliminary diagnosis. In order to finally approve the presence of the etiology of the plague, a pure culture of the pathogen is isolated and identified.
plague treatment

Treatment of patients can take place exclusively in a hospital. Preparations for etiotropic therapy, their doses, and treatment regimens are determined depending on the form of the disease. Usually the course of therapy is from 7 to 10 days, regardless of the form of the disease. In this case, the following drugs are used:
skin form – cotrimoxazole (4 tablets per day);
the bubonic form is levomycetin (dose: 80 mg/kg per day) and streptomycin is simultaneously used (dose: 50 mg/kg per day). The drugs are administered intravenously. The effectiveness of tetracycline has been noted;
pulmonary and septic forms – a combination of chloramphenicol with streptomycin + doxycycline (dose: 0,3 grams per day) or tetracycline (4-6 g / day), taken orally.
Along with this, massive detoxification therapy is carried out: albumin, fresh frozen plasma, rheopolyglucin, intravenous crystalloid solutions, hemodez, extracorporeal detoxification methods. Prescribed drugs that improve microcirculation: picamilon, trental in combination with solcoseryl. Forcing diuresis, cardiac glycosides, as well as respiratory and vascular analeptics, symptomatic and antipyretic drugs.
As a rule, the success of the treatment depends on how timely the therapy was carried out. Etiotropic drugs are usually prescribed at the first suspicion of plague, based on clinical and epidemiological data.
Plague prevention
Epidemiological surveillance
The forecast of the epidemic and epizootic situation in individual natural foci determines the nature, direction and scope of measures to prevent the disease. This takes into account data obtained from monitoring the growth in the number of people infected with plague around the world. All countries should report to WHO on cases of plague, movement of infection, epizootics among animals, as well as measures taken to combat the disease. Usually, a system of passportization is developed in the country, which fixes the natural foci of the plague and allows for the zoning of the territory in accordance with the scale of the epidemic.
Preventive measures
The leading role in the complex of preventive measures is played by measures that prevent the importation of infection from other countries, as well as preventing the development of plague in enzootic foci. In order to prevent the importation of infection, international sanitary rules have been created. And in enzootic foci, the number and species composition of rodents are monitored, and animal studies are carried out in order to detect infection. If an epizootic has been detected, then deratization and various pest control measures are carried out. Synanthropic rodents are exterminated without detection of infected individuals, if more than 15% of those caught in traps are infected. Rodents and ectoparasites on the plains and near human settlements are being destroyed by special anti-plague facilities, and in the settlements themselves by departments of the Center for Sanitary and Epidemiological Surveillance.
If an epizootic of plague in rodents is noticed or cases of the disease are detected among domestic animals, and also if the infection is likely to be imported by an infected person, preventive immunization of the population is carried out. Vaccination can be carried out without exception or selectively – to individuals who have a connection with those territories where the epizootic exists (hunters, agronomists, geologists, archaeologists). All health care facilities should have a stock of medicines, as well as protective and preventive equipment, and a scheme for communicating information and alerting staff should be developed. Preventive measures in enzootic areas, as well as for persons who are in contact with pathogens of dangerous infections, are carried out by various anti-plague and many other public health institutions.
Activities in the epidemic focus
If a case of plague has been identified, or there is a suspicion that a person is a carrier of this infection, urgent measures must be taken to localize and eliminate the outbreak. Based on the epidemiological or epizootological situation, the size of the territory on which restrictive measures – quarantine should be introduced – is determined. Also taken into account are possible operating factors through which the infection can be transmitted, sanitary and hygienic conditions, the number of migrating people and transport links with nearby territories.
The Extraordinary Anti-Epidemiological Commission supervises the activities in the area of the focus of infection. The anti-epidemic regime must be strictly observed, the commission employees must use protective suits. The Extraordinary Commission makes a decision regarding the introduction of quarantine throughout the outbreak.
Specialized hospitals are being set up for plague patients and those with suspicious symptoms. Infected people are transported in a strictly defined manner, in accordance with the current sanitary rules for biological safety. Those infected with bubonic plague can be accommodated by several people in one ward, and patients with the pulmonary form must be distributed in separate rooms. It is allowed to discharge a person who has had bubonic plague at least 4 weeks after the moment of clinical recovery (presence of negative results of bacteriological tests). With pneumonic plague, a person must be in the hospital after recovery for at least 6 weeks. After the patient leaves the hospital, he is followed up for 3 months.
The focus of infection is subject to thorough disinfection (current and final). Those persons who came into contact with infected people, their belongings, corpses, as well as participants in the slaughter of sick animals, are isolated for 6 days and are subject to medical supervision. In the case of pneumonic plague, individual isolation for 6 days is necessary for all persons who could become infected, and provide them with prophylactic antibiotics (rifampicin, streptomycin and the like).









