Contents
What is cervical dysplasia?
cervical dysplasia (cervical dysplasia) is a condition of the epithelium covering the cervix, which is characterized by a change in the number of layers and the structure of the cells that form it. At the same time, the basement membrane and the uppermost cell layers are not involved in the process. Dysplasia refers to diseases that, under certain circumstances, can cause the development of a malignant tumor of the cervix.
Cervical dysplasia is an extremely dangerous pathology and the most common precancerous form that changes the structure of the mucous membrane of the cervix and vagina. Dysplasia can have a different origin, but it is always accompanied by a violation of the cellular structure of the epithelium. It affects not only the upper layers, but can penetrate much deeper.
Often cervical dysplasia is called erosion, but this term does not fully convey the essence of the phenomenon. The main difference between these two processes is that erosion occurs due to mechanical damage to tissues, and dysplasia is characterized by a violation of the cellular structure of tissues.
Depending on the depth of damage to the mucous membrane of the cervix, there are:

a mild (mild) form of dysplasia (up to a third of the thickness of the layers of the squamous epithelium is affected; the cells of the intermediate layer may swell);
moderately pronounced (medium) form of dysplasia (from one third to two thirds of the thickness is affected; the polarity of the epithelium is disturbed);
a pronounced (severe) form of dysplasia (all layers of the epithelium are affected).
Every year, about 40 million women in the world are diagnosed with cervical dysplasia for the first time or confirmed. This disease accounts for approximately 15-18% of cases of identified pathologies of the cervix. It is typical for women in the reproductive age of 34-35 years. The average frequency of transition of severe forms of cervical dysplasia to cancer is approximately 10-30% according to various studies.
Most patients, not understanding the essence of the pathological mechanisms, confuse cervical dysplasia with erosion or a cancerous tumor. Neither statement is correct. To understand what the difference is, you need to turn to anatomy.
Dysplasia from a doctor’s point of view

The cervix is the boundary between the vagina and the uterus itself. It consists of 3 types of fabrics:
epithelial;
muscular;
connecting.
A feature of its epithelium is that it is heterogeneous in its structure. The cervix is the meeting point of 2 types of integumentary epithelium: cylindrical, the cells of which are located in one layer, have a rectangular shape and line the uterine cavity and cervical canal, and stratified squamous, characteristic of the vagina and represented by several rows of flattened cells. Both epithelium is located on a thin basement membrane, consisting of collagen fibers and playing the role of a strong foundation and limiter.
It is precisely because of such a complex structure of the cervix that various pathological processes often occur in this area associated with changes in cell characteristics.
The most basic of them are:
Erosion – this is a displacement of the cylindrical epithelium towards the vagina. The structure, functions, features of cell growth are not violated. Due to the difference in conditions in the cervical canal and in the vagina, cylindrical cells are damaged by an acidic environment, waste products of the normal microflora of the female genital tract, trauma during intercourse, forming poorly healing wounds – erosion. During a gynecological examination on a chair, it looks like a patch of rich red on a pale pink background.
Cervical cancer – this is a process of changing the structure, functions of epithelial cells, which have acquired the ability to unlimited growth. If the overgrown cells have not gone beyond the basement membrane, then they speak of “cancer in situ” (CIS carcinoma in situ), it is the initial stage in the development of malignant neoplasms of any internal organs. If a cancerous tumor has grown through the basement membrane, then from a medical point of view, we are talking about invasive cancer (this is cancer in the layman’s sense).
Dysplasia – this is a change in the structure of the stratified squamous epithelium that covers the cervix, while cells with an “abnormal” shape of the nucleus appear in it, multinucleated, irregular in shape, the anatomical division into layers is lost. However, the altered cells do not have the ability to grow indefinitely and do not penetrate beyond the basement membrane. The cylindrical epithelium in the transition zone on the cervix remains unchanged.
Modern medicine has not used the term “dysplasia” for a long time, instead of it, both in the diagnosis and in the scientific literature, you can find the following definition: cervical intraepithelial neoplasia (CIN, or CIN), which means the formation of new cellular elements of the cervical epithelium that are not characteristic of this tissue.
Causes of cervical dysplasia
The appearance of cervical dysplasia, like any other precancerous disease, does not occur under the influence of any one factor. It is always a complex combination of many provoking components.
The main reasons for the formation of foci of dysplasia are:
infection with certain types of human papillomavirus (HPV);
hormonal contraceptive pills for long-term use (from 5 years);
early onset of sexual activity (14-15 years);
a large number of sexual partners;
bad habits (smoking).
Also, their role in the development of dysplastic processes can have:
monotonous diet with a lack of vitamins C, A;
immunity disorders;
genetic predisposition to any oncological diseases;
genital infections;
low level of education, life, antisocial behavior;
a large number of births.
The discovery of the dominant role of the HPV virus in the development of dysplasia and malignant tumors of the cervix was a breakthrough in the development of effective methods to combat cancer of the female reproductive system.
Viral factor
Cervical dysplasia most often develops due to human papillomavirus (HPV). This disease is most often asymptomatic, from the onset of dysplasia to the onset of cervical cancer, it usually takes about 10 years.
Anyone can become infected with the human papillomavirus, but women who are sexually active and have multiple sexual partners are at risk. Neglect of contraception and untreated inflammation of the organs of the reproductive system also increase the likelihood of contracting HPV. Injury to the cervix can also occur due to abortions or frequent births.
There are a large number of HPV virus types, each of which can cause characteristic lesions. For example: common warts on the arms and legs, genital warts in the genital area; dysplasia and cervical cancer.
According to the degree of oncological “danger”, all types of HPV can be divided into 3 categories:
Non-oncogenic and low oncogenic risk types are found in warts and genital warts, these are types 1, 2, 3, 5, 6, 11, 42, 43, 44.
Low oncogenic risk. Viruses belonging to highly oncogenic serotypes are found in 90% of all cases of dysplasia and malignant neoplasms of the cervix. These are 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68 types.
high oncogenic risk. Particularly aggressive of them are 16 and 18, which are more common than others and lead to the development of cervical cancer in half of the cases.
How does HPV cause cellular changes?
In a healthy body, any damaged cell is immediately destroyed by the immune system and internal antitumor mechanisms that do not allow it to enter into the process of division and reproduce similar defective cells. In addition, the number of divisions of each cell type is strictly limited by the genetic program. This determines the aging process in the body, with all the desire a person cannot live forever.
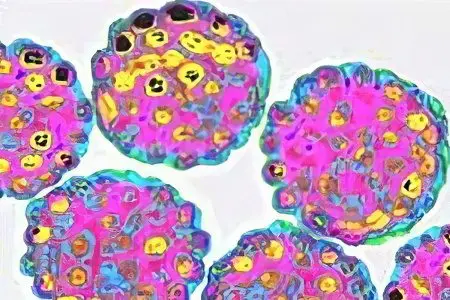
When the HPV virus, which has a high oncogenic activity, enters the body, it is carried by the blood to the genitals and embedded in the cells of the squamous cervical epithelium. Viral particles produce special proteins that block the “security system” of the epithelial cell and damage DNA. As a result, atypical cells are formed that do not die, are not removed by the immune system, they are capable of dividing and reproducing similar “abnormal” specimens to themselves. Thus, there is a change in the structure of the layers of the epithelium of the cervix, which in the analysis is defined as cervical intraepithelial neoplasia (CIN, or CIN). However, in dysplasia, unlike cancer, atypical cells do not have the property of unlimited uncontrolled growth.
Contraceptive use
The influence of long-term use of hormonal combined oral contraceptives (COCs) on the occurrence of dysplastic processes in the cervix has been well studied.
In this case, 2 separate effects (COCs) take place:
mediated;
straight.
Indirect effect is that women who constantly take COCs, usually young aged 20-40 years, are sexually active, often change sexual partners, they suffer from venereal diseases more often than others in the population, and smoke. The combination of these factors increases the risk of developing dysplastic processes in the cervix.
Direct effect mechanism has not been fully studied, however, based on statistical data, it was concluded that long-term use of COCs (5 years or more) increases the risk of developing cervical dysplasia by almost 2 times.
Women who use progestin drugs (birth control pills for pregnant women) for protection do not fall into the risk category, since this type of contraceptive does not affect the cervical epithelium. The same applies to women in menopause or with ovaries removed who receive hormone replacement therapy, the risk of developing dysplastic processes does not increase in them.
Other reasons
The causes of cervical dysplasia can be both an unhealthy lifestyle and bad habits (especially smoking), since reduced immunity and hypoxia increase the likelihood of microtrauma of the cervical epithelium.
Other reasons, such as early sexual activity, a large number of sexual partners, low social level – all of them are directly related to the frequent infection of this category of women with various types of HPV.
Lack of vitamins A and C, immunodeficiency states, genetic predisposition lead to a violation of the body’s defense system and failures in the program for the destruction of damaged cellular elements, which also contributes to the development of dysplastic processes.
In general, the development of cervical dysplasia can be explained using the theory of “weeds”, which was proposed in 1995 by a professor at the University of California, a gynecologist Michael Policar (Michael Policar). In his opinion, the cervical epithelium is the soil where the “seeds” of cellular changes in the form of HPV fall, however, in order for them to germinate, “water, light, heat” are needed, the role of which is played by other factors in the development of dysplastic processes – smoking, decreased immunity , beriberi, genetic predisposition. Without them, even in the presence of HPV, the development of cervical dysplasia does not occur.
To date, this theory has not been clinically and laboratory confirmed. However, the combination of HPV with other risk factors in most women supports this scientific hypothesis.
Symptoms of cervical dysplasia

In the initial forms, the disease is often asymptomatic. The disease manifests itself only in advanced conditions: a woman has pain in the lower abdomen, there may be mild vaginal bleeding. To avoid this and start treatment on time, it is necessary to undergo regular gynecological examinations, which include instrumental, laboratory and clinical studies.
Signs of dysplasia can only be detected if the symptoms are accompanied by other diseases. According to gynecologists, in most cases, in the presence of cervical dysplasia, there is erosion of the cervix. Therefore, a competent doctor will certainly refer the patient to the PAP analysis (SMEAR) if erosion is detected in her.
Symptoms of dysplasia may include:
copious leucorrhoea without an unpleasant odor, milky white;
streaks of blood in vaginal discharge after intimacy;
pain during sexual intercourse.
Once again, it must be repeated: these symptoms are not specific to cervical dysplasia, cannot be used for diagnosis, but are only a reminder to the woman that her women’s health needs a thorough examination.
Degrees of dysplasia
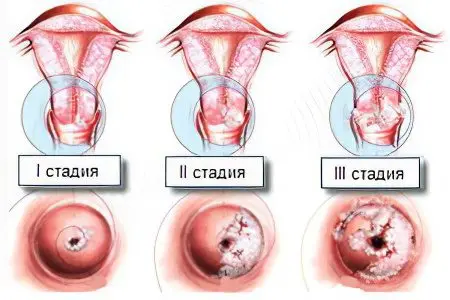
Depending on how deeply the cervical epithelium is affected, there are 3 degrees of cervical dysplasia:
1 degree (weak);
2 degree (moderate);
3 degree severe.
If we imagine a section of the epithelium in the form of a rectangle, the lower side of which is represented by the basement membrane, and the upper side is the surface row of cells, then the various degrees of dysplasia will look like this.
Cervical dysplasia grade 1 (weak)
In medical documentation (test results or discharge), it is designated as follows: CIN I (cervical intraepithelial neoplasia I). It is placed in the event that only the lower 1/3 of the epithelial layer adjacent to the basement membrane has undergone pathological changes.
Cervical dysplasia grade 2 (moderate)
The diagnosis is referred to as CIN II (cervical intraepithelial neoplasia II). It is established when the pathological process spreads to 2/3 of the depth of the epithelium, while the upper 1/3 remains unaffected.
Cervical dysplasia grade 3 (severe)
Referred to as CIN III (cervical intraepithelial neoplasia III). It is the most severe form of cervical dysplasia, when the structure of all layers of the epithelium is disturbed. This degree is a fine line between dysplasia per se and the initial stage of cancer (“cancer in situ”, or carcinoma in situ). In neither case does the basement membrane remain intact. All the difference is only in the function of cells, which acquire the ability to divide indefinitely. Histological examination can help to establish the severity of the pathological process.
Consequences of cervical dysplasia
What can threaten a woman with cervical dysplasia directly depends on its degree:
1 degree
Cervical dysplasia of the 1st degree in 57% of cases resolves on its own after the removal of the virus from the woman’s body. In a healthy person, in 9 cases out of 10, the virus ceases to be detected in blood tests after six months or a year from the moment it enters the body. There is an independent destruction of viral particles by the immune system.
2 degree
Cervical dysplasia of the 2nd degree in 43% of cases also goes away on its own after the release of the body from HPV. In 35%, its long-term stable course is observed. Thus, 70% of women recover after 2 years from the moment of diagnosis.
3 degree
According to studies conducted among various categories of women, the probability of transition of the 3rd degree of cervical dysplasia to cancer is 10-30%. The reason for this scatter of results is the presence of a different number of individual risk factors in different categories of women (by age, contraceptive methods, bad habits, lifestyle, number of sexual partners).
Cervical dysplasia and pregnancy

Cervical dysplasia does not apply to contraindications to bearing a fetus in women who were first diagnosed during pregnancy. The presence of this pathological process does not affect the development of the unborn child, does not inhibit the function of the placenta. At the same time, pregnancy itself does not in any way affect cervical dysplasia, does not worsen its course and does not contribute to the transition to a more severe form.
In addition, under the influence of hormonal changes that occur in a pregnant woman, physiological changes can develop on the cervix that can be mistaken for cervical dysplasia. We are talking about ectrapion (pseudo-erosion), in which the cells characteristic of the cervical canal are shifted towards the vagina. On examination, this condition is defined as a red corolla on the cervix.
Therefore, if a woman was examined for 1-3 years before pregnancy and has a negative result of a cytological analysis, then a second control is not assigned.
If a pregnant woman has never been examined either for HPV carriage or for atypical cells, then when changes are first detected on the cervix, a smear is taken for a Papanicolaou study (smear-test) at any time.
Further tactics depend on the result. If it is negative, then no further action is taken and control is assigned 12 months after delivery. If the test is positive and a mild degree of dysplasia is detected, then colposcopy and control are performed 12 months after birth.
With an average degree of cervical dysplasia, colposcopy and re-examination after childbirth are prescribed.
If grade 3 dysplasia is suspected, a targeted biopsy is performed – taking a piece of altered tissue for analysis. If severe dysplasia is confirmed, colposcopy should be performed every 3 months until the very birth and the first 1,5 months from the moment of delivery.
If cancer is detected, further management of the patient is agreed with the oncologist and depends on the specific situation.
Diagnosis of cervical dysplasia

Since dysplasia can turn into cancer under a number of conditions, the most important thing in preventing complications is its early diagnosis. All women over 21 who are sexually active should visit a gynecologist once a year for an examination and undergo a cytological examination once every 1 years.
The following common methods are used in the diagnosis of this disease:
inspection;
cytological examination of a smear (according to Papanicolaou, or smear-test);
colposcopy;
taking a piece of tissue (targeted biopsy).
When viewed in mirrors, areas of dysplasia look like irregularly shaped areas (plaques) of a whitish color. When carrying out the Schiller test – staining the cervical epithelium with Lugol’s solution – uneven staining is determined. Areas of dysplasia remain lighter than healthy tissue.
Colposcopy is an instrumental method of examining the vaginal part of the cervix with a special magnifying device – a colposcope. On examination, incorrectly located branched blood vessels in the area of dysplasia, mosaicism, and pale color of the altered epithelium will be visible. When treating the cervix with a solution of acetic acid, the changed areas will be white.
It should be remembered that none of these methods can differentiate a severe degree of dysplasia from cancer. This is possible only with the help of a histological examination of a piece of epithelium. The method by which this is done is called a targeted biopsy with curettage of the cervical canal. The tissues obtained as a result of the procedure are carefully studied. This method has 100% accuracy.
Treatment of cervical dysplasia

Before treating cervical dysplasia, the doctor detects and eliminates its cause (hormonal disorders, infections or inflammation). This should stop the development of dysplasia in undeveloped forms and contribute to tissue scarring. In other cases, patients are recommended surgical treatment.
A common method of treating dysplasia is an electroknife, which is used to excise the affected tissue. Healing after such an operation takes three months, but scarring and bleeding are possible, which creates the risk of an unfavorable course of pregnancy.
Also, cervical dysplasia is treated with laser surgery. Depending on the neglect of the pathological process, healing can take about two months, but this treatment is safe and passes with virtually no consequences.
Another method of surgical treatment of dysplasia is cryotherapy. Affected tissues are frozen with liquid nitrogen. In addition, there is also a chemical method of treatment, which consists in applying a special chemical preparation that cauterizes tissues to the foci of dysplasia. After a couple of days, they fall off in the form of a thin crust.
The severity of the pathological process affects the tactics of treatment:
1 degree
Since there are scientifically confirmed data that in most cases cervical dysplasia of the 1st degree goes away on its own after 1-2 years, provided that the body is freed from HPV, modern doctors do not recommend using any treatment at this stage.
The treatment strategy is as follows:
dynamic observation up to 2 years from the moment of diagnosis;
analysis for cytology and colposcopy every year;
treatment of diseases of the reproductive system (vaginitis, venereal infections);
the fight against bad habits (cessation of smoking);
selection of alternative methods of contraception;
correction of disorders of the endocrine system.
Since antiviral drugs for the treatment of HPV have not yet been created, proper nutrition and vitamin support are of great help to the body in the fight against the virus. It is recommended to take multivitamin complexes containing vitamins E, B12, B6, A, C, folic acid, selenium.
If during the control examination, carried out 2 years after the diagnosis, there is no tendency for grade 1 dysplasia to decrease, or, conversely, there are signs of its transition to grade 2, then it becomes necessary to use more aggressive methods of treatment.
Small areas of cervical dysplasia of the 1st degree are successfully treated by treating them with a drug for chemical coagulation such as Solkogin, Vagotid.
2nd and 3rd degree
For the treatment of grades 2 and 3 of cervical dysplasia, surgical methods are used:
Cauterization
Cryodestruction
Laser treatment
Radio wave treatment
Electroconization (excision)
Photodynamic therapy
Surgical treatment should be carried out immediately after the end of menstruation, this prevents the development of endometriosis and improves the healing process. Before the procedure, it is necessary to take smears for cytological examination, colposcopy and biopsy.
Ignition:
Operating principle cauterization is based on the fact that pathologically altered cells are destroyed under the influence of a low voltage current. The procedure is performed using a special apparatus with electrodes in the form of a loop.
Advantages of the method is its low cost, availability of equipment, technical ease of implementation.
Disadvantages of the technique: the inability to control the depth of exposure, rough scars after healing, there is a high risk of developing complications in the form of endometriosis.
Cryodestruction:
With this method, the removal of altered epithelial cells is carried out by instant freezing them with liquid nitrogen. The temperature of liquid nitrogen is -196 C%, the water contained in the epithelial cells instantly turns into ice, thus the altered tissue areas die.
Advantages of the method in that it does not leave behind rough scars, therefore it can be recommended to nulliparous women if it is impossible to use more technological methods.
disadvantages include abundant clear discharge after the freezing procedure, which can disturb a woman for up to 1 month, the need to refrain from sexual intercourse for up to 2 months from the time of treatment, the inability to adequately control the depth of processing.
Laser treatment:
This method is based on the “evaporation” of affected tissues under the action of laser energy.
Advantages: does not leave rough scars, modern equipment allows you to control the depth of penetration of the laser beam, which allows you to completely remove all the pathological tissue.
Disadvantages: burns of adjacent healthy areas of the cervix may occur, short-term anesthesia may be required, since the effectiveness directly depends on the immobility of the patient.
Рadiowave treatment: Refers to relatively new techniques, it is based on the removal of a focus of dysplasia under the influence of high frequency waves. It is performed on the Surgitron apparatus.
The advantages of the method are:
low trauma;
the ability to control the depth of impact;
painlessness;
short rehabilitation period;
absence of rough scars after the healing period;
a small percentage of recurrence of areas of dysplasia;
the ability to use in nulliparous women.
Disadvantages: a very expensive method, which is available only in private clinics.
Excision (conization): removal of areas of dysplasia with a scalpel or Surgitron apparatus. Due to the high trauma and a large number of complications after the procedure, it is not used in women of childbearing age. Currently, instead of conization with a scalpel, conization with a laser beam is used. With such an operation, the likelihood of bleeding both during the procedure and during the rehabilitation period is reduced, which is associated with the cauterizing effect of the laser.
Read more: Electroconization of the cervix for dysplasia
Photodynamic therapy: is one of the newest methods of treatment of oncological diseases. Its essence is reduced to the selective accumulation of a photosensitizer by the tumor after intravenous or local administration. Subsequently, the cancerous tumor is irradiated with a light source (laser or non-laser). As a result, a reaction occurs in the affected tissues with the release of singlet oxygen. This leads to the death of cancer cells.
Read more: Photodynamic therapy of the cervix
With any method of treatment in the postoperative period, it is necessary to adhere to a certain regimen during the first month:
Sexual rest;
Do not lift weights;
Do not play sports;
Do not visit the pool, sauna, beach;
Do not sunbathe or go to the solarium, especially in women infected with HPV;
Do not take a bath, only a shower is allowed;
Do not inject into the vagina any drugs, solutions, except those prescribed by a doctor;
Be sure to conduct a control gynecological examination after the next menstrual cycle after treatment.
Many women, fearing to hear the diagnosis, put off a visit to the gynecologist, but this is a false fear. Cervical dysplasia is perfectly treatable if done on time and with the right method.
Medications

If the diagnosis of cervical dysplasia was carried out in the early stages, then getting rid of the disease in most cases is successful. Taking drugs is prescribed as an auxiliary therapeutic measure, and surgery is considered to be the main method of treatment. During its implementation, pathological areas are removed. However, drug correction is still required. First of all, it is necessary to neutralize HPV, which very often leads to the development of dysplasia. The choice of drugs should be based on the individual characteristics of the course of the disease, it should also be based on the age of the patient and her desire to have children in the future.
The objectives of the therapy are as follows:
Relieve inflammation (anti-inflammatory drugs).
Restore the functioning of the epithelial tissue (hormonal preparations are prescribed).
Increase the body’s resistance (immunomodulators).
Restore the microflora of the vagina.
So, at the stage of drug correction, immunomodulators, vitamin-mineral complexes (vitamins A, C, E, folic acid) are prescribed.
Preparations for the treatment of cervical dysplasia
Preparations for stimulating immunity |
|
|
Vitamins and minerals |
|
|
Doctors, if possible, try to delay surgery for as long as possible. However, it is not always possible to cope with cervical dysplasia with the help of medications. Therefore, in 65-70% of cases, you still have to resort to the help of a surgeon. In the future, medical correction is prescribed.
Antibiotics and antiviral agents are prescribed only when dysplasia is severe. In general, drug therapy in neoplastic processes is ineffective.









