Contents
Dystrophic processes and dysfunction of the intervertebral discs of the cervical spine are called cervical osteochondrosis (COX).
What is cervical osteochondrosis?
Cervical osteochondrosis – This is a disease in which the soft intervertebral pulp, which acts as a shock absorber between the vertebrae, degenerates into ossified tissue, while nerve roots and blood vessels are involved in the pathogenesis. This pathology masquerades as a variety of disorders. A distinctive feature of osteochondrosis of the cervical spine is pain in the head, neck and upper back. Also, patients go to the doctor with dizziness, nausea, jumps in blood pressure, loss of consciousness, lack of air, numbness of the tongue, suspected angina pectoris and other pathologies of the cardiovascular system.
This means that a person who feels pain in the back of the head, shoulders, arms, sternum and in the retrosternal region complains not only to a neurologist, but also to doctors of other medical specialties (cardiologist, general practitioner, orthopedist), which seriously complicates the initial diagnosis of the disease. .
Dystrophic changes in the tissues of the cervical spine are widespread among middle-aged and older people. This is due to the vertical arrangement of the human skeleton and the distribution of static and dynamic loads.
The wide distribution of cervical osteochondrosis is explained by the peculiarities of the exit of the roots of nerve endings in the upper part of the spinal column and the mobility of the neck joints, which bear the load of keeping the skull in an upright position.

In modern society, neck osteochondrosis is being rejuvenated. When examining representatives of different generations with a tendency to this disease, it was reliably established that today’s youth begin to experience difficulties with the spine much earlier in comparison with the representatives of the older generation of the family, sometimes even in adolescence. People born 60-70 years ago first go to a medical institution for cervical osteochondrosis in adulthood or even in old age, but people born 20-40 years ago often get osteochondrosis at a young age. This indicates a significant deterioration in the health of the younger generation, which is associated with a sedentary lifestyle and a decrease in the quality of nutrition.
osteochondrosis It is customary to consider in two ways, always in the relationship of physiological (natural aging of the body) and pathological (dystrophic and inflammatory processes) factors:
Physiological process – the inevitable aging of the cartilage of the spinal column, regulated by the neuro-endocrine mechanisms of the body as a result of natural irreversible phenomena;
Pathological process – destruction of the intervertebral structures and the nerve nodes and blood vessels surrounding the vertebrae – the less healthy the lifestyle, the faster the disease develops.
From the point of view of the localization of the pathological process:
Physiological changes are located in the center of the intervertebral disc, are accompanied by replacement of the pulp of the disc with fibrous tissue, are part of the aging process of the body, are not clinically manifested or appear only when the nerve endings are irritated;
Pathological changes spread outside the cartilage, always cause irritation of nerve endings and compression of blood vessels, which is manifested by local and reflected pain reactions (dyscalgia).
The pathological form of osteochondrosis is the replacement of physiological aging with a pathological process.
The disease can be eliminated on its own, compensated and manifest itself episodically. This feature is associated with the ability of the organism of higher mammals and humans to develop compensatory and protective mechanisms that level pathology. Meanwhile, it is inappropriate to test the body for strength.
The pathological form of the disease is always associated with the aging of the body, even in young people. Further destruction of the tissues of the fibrous ring without replacement of the pulp with fibrous tissue leads to the formation of microcracks, impaired fixation of the vertebrae, and the development of symptoms of spinal instability.
The pathogenesis is accompanied by:
Impregnation of the nucleus pulposus with calcium salts;
By pressing the structures of a vertebra into the body of an adjacent vertebra (like a hernia);
Gradual wear of the vertebrae (spondylosis);
Ossification of ligaments (ossifying ligamentosis).
Symptoms of cervical osteochondrosis

Diagnosis of the disease is difficult, pain is sometimes not manifested, and the symptoms are blurred, in addition, the uncontrolled use of strong analgesics masks the signs of the disease. A patient who does not feel pain considers himself healthy, and this continues until the development of irreversible processes in the tissues of the neck joints.
Important symptoms of cervical osteochondrosis are dizziness, headaches, jumps in blood pressure.
Dizziness with cervical osteochondrosis
This condition does not always clearly indicate osteochondrosis of the cervical spine.
Dizziness may be due to:
Inflammation in the middle or inner ear;
Spasms of cerebral vessels;
Violations of the transmission of nerve impulses;
Problems with the vestibular apparatus;
Diseases of the cardiovascular system.
There are no clear criteria for dizziness in osteochondrosis. However, there are systemic and non-systemic dizziness, they have clear differences.
It is recommended to know the differences between systemic and non-systemic dizziness, this will help to independently determine the causes of an unusual condition:
Systemic dizziness – this is a feeling of circular movement of surrounding objects or the body, which is a consequence of a violation of the vestibular apparatus, visual analyzers and receptors in the joints, muscles and epidermis (osteochondrosis of various etiologies);
Unsystematic vertigo – this is a feeling of dizziness, a feeling of stupor, an insecure state in an upright position. With non-systemic dizziness, there is no sensation of circular rotation, and this is an important difference between the compared signs.
A person who feels dizziness of one of these types should be examined by an experienced doctor, first of all, by a neuropathologist or (if there is a suspicion of an ear and nasopharyngeal disease) by an otolaryngologist.
The reason for emergency hospitalization, not associated with osteochondrosis of the cervical spine, is the identification in the patient (except for dizziness) of such signs as:
Paralysis of the facial muscles and numbness of part of the shoulder girdle;
Severe headache against the background of deterioration of health;
Disturbances in coordination of movements;
Loss or extinction of consciousness.
Headache with cervical osteochondrosis
This is one of the most common non-specific signs of many human diseases. Headaches are especially widespread in the female population. It can be difficult to determine the cause of headaches, and, even more so, to associate it with spinal lesions. About 14 different causes of headache in humans have been identified.
The most common causes of headache in the pathology we describe are:
Spasms of cerebral vessels;
Pinched nerve roots;
Reflex increase in intracranial pressure.
Headache in cervical osteochondrosis may resemble sensations in arterial hypertension, angina pectoris or stroke. Moreover, people of middle and older age, as a rule, have risks of developing strokes or heart attacks.
The pain can feel like paroxysmal, constant, throbbing and dull.
With pathologies of the heart, patients complain of discomfort in the chest area, accompanied by a violation of the rhythm of cardiac activity. Only a qualified doctor can determine the cause. In the event of headaches, combined with nausea, dizziness and retrosternal pain, an ECG is mandatory.
Pain in osteochondrosis of the cervical region

Not always the pain is localized in the head and neck. Cases of other localization of pain are known.
Neck pain (cervicalgia) can radiate to the shoulder area and to various parts of the arms. A distinctive feature of such sensations is the suddenness of seizures after sleep, sudden movements, and tensions that are hardly noticeable to a person, for example, when laughing or sneezing. The pain associated with osteochondrosis, if the process has not become chronic, usually subsides after some short time and is combined with a crunch in the cervical vertebrae.
Without a preliminary examination, pain should not be relieved with manual therapy (massage). In some cases, inept manipulation can only aggravate the pathology, disrupt the innervation and lead to the patient’s disability.
The intensity of the pain can be moderate or severe. By duration – both short and long.
Typical sensations described by patients:
Localization of pain in the depth of the neck;
Sensation of crunching and crackling when you try to turn your head;
Muscle weakness or decreased sensation in different parts of the body.
In the cervical region of all mammals, including humans, there are seven vertebrae and eight pairs of ganglions. MOC can also develop at the border of the cervical and thoracic vertebrae.
It is noted that osteochondrosis of the cervical region is most often associated with lesions of the sixth and seventh cervical vertebrae.
There are tests to determine the localization of the focus of the pain impulse. A lesion in the region of the sixth vertebra is accompanied by pain in the thumb, and a lesion in the region of the seventh vertebra is accompanied by pain in the middle finger.
Blood pressure in cervical osteochondrosis
The connection of cervical osteochondrosis with jumps in blood pressure has long been established. The cervical vertebrae have important nerve endings and blood vessels.
Characterized by pressure surges during the day. Hypertension for a long time is not characteristic of this disease. Reflex irritation of nerve endings and short-term spasms of blood vessels cause spasmodic daily dynamics of arterial hypertension.
A distinctive feature of high blood pressure in cervical osteochondrosis is a combination with the following symptoms:
Headache;
Pain in limbs and chest;
Decreased sensitivity in the area of the collar zone;
The occurrence of pressure surges after stress, muscle tension, prolonged exposure to an uncomfortable position and other similar situations.
These signs should be taken into account in self-differentiation of hypertension of various origins.
Sharp jumps in blood pressure and a rapid deterioration in well-being are the basis for seeking emergency medical help.
Causes of cervical osteochondrosis
The reasons are always associated with the aging of the body and the developed pathology of bone and cartilage tissue. However, not all people in old age suffer from various types of skeletal pathologies.
Numerous observations have established that cervical osteochondrosis has provoking factors, including:
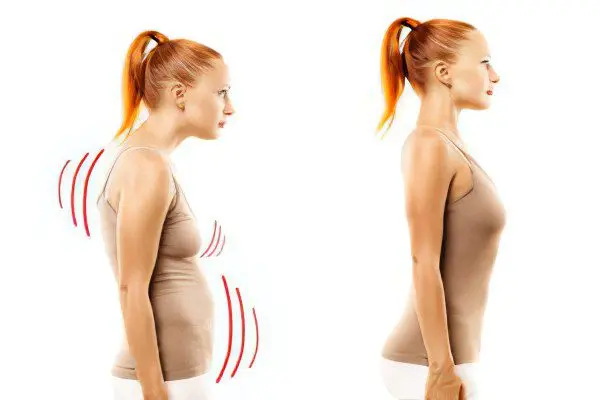
Sedentary lifestyle;
Forced postures in the process of work;
Excess body weight;
Excessive nervous tension and prolonged stress;
Previous injuries in the back of the head and neck;
Local hypothermia;
Autoimmune diseases that lead to cartilage degeneration;
Congenital anomalies in the structure of the spine.
Moderate physical activity, a healthy diet and a proper lifestyle significantly reduce the risk of osteochondrosis, or minimize its impact on well-being in old age.
Why is cervical osteochondrosis dangerous?
Decreased flexibility in the joints, muscle elasticity and other signs of aging of the body – unconditional companions of the elderly – is a natural process.
Pain during movement and at rest begin to annoy a person much earlier than the natural aging period, sometimes it ends with disability or a significant decrease in the quality of life.
Inept treatment is just as dangerous as inaction, because in the first case, the pathology worsens without quality treatment, in the second, inept therapy can result in sudden disability or a persistent deterioration in well-being, because medical manipulations affect the two most important body systems – nervous and vascular.
Syndromes of cervical osteochondrosis
Syndromes are a combination of several symptoms. There are several symptom complexes of cervical osteochondrosis, the main ones are:
Vertebral or vertebral;
vertebral artery;
Cardiac or cardiac;
Nerve endings (radicular).
The combination of different syndromes, like a mosaic, develops into a single picture of cervical osteochondrosis.
Vertebral syndrome
This syndrome means that pathological processes are associated with the body of bone and cartilage tissue.
In the case of clinical manifestation, the syndrome consists of three symptoms associated with damage to the bone or cartilage tissue of the vertebrae, namely:
Impaired mobility of the neck;
Pain when trying to turn the neck;
Morphological changes in the vertebral body or in the intervertebral space (the symptom is determined on the x-ray).
These symptoms must be combined with each other. In the absence of one of them, there is also no vertebral syndrome – this is a medical axiom. In the presence of pain during head rotation, morphological changes in the tissues of the bones and cartilage of the cervical skeleton can always be assumed, and by indirect signs (change in the place of sensitivity), it is possible to determine a specific vertebra or group of joints involved in the pathology.
The complexity of diagnosing vertebral syndrome lies in the fact that a similar clinical picture (restriction of neck mobility) can also be detected with lesions of the neck muscles (myositis), and the main symptom of the syndrome – pain with an active change in the position of the neck – is often the result of other pathological processes in the human body.
Syndrome of the vertebral artery
This syndrome means that pathological processes are associated with the vertebral arteries that supply the brain. The manifestation of symptoms should be considered in direct connection with a violation of the blood supply to the brain and tissues of the cervical region.
The syndrome consists of several symptoms. The main ones are related to:
Insufficient blood flow in one of the trunks due to arterial compression (tinnitus, state of stunning, dizziness, pressure surges, nausea and vomiting);
Irritation of the nerve endings of the artery (severe pain and migraine, or vice versa, numbness, decreased sensitivity, temporary one-sided blindness or “flies” in the eyes);
Oxygen starvation (drowsiness, fainting, mild aching headache, decreased performance and concentration, depression).
This syndrome can develop not only with osteochondrosis, but also with other pathologies (deposition of atherosclerotic plaques on the inner wall of blood vessels, squeezing of the vessel by tumors, inflammatory infiltrate, and so on).
Cardiac syndrome
Signs of this syndrome resemble cardiac disorders, angina pectoris, and even a condition preceding a heart attack. The syndrome includes the following symptoms:
Pain and burning in the chest area;
Shortness of breath, weakness and fatigue;
Cardiopalmus.
The main methods of differential diagnosis of pathologies of the cardiovascular system and osteochondrosis are the ECG method and functional tests. On the ECG, a shortened ST segment is noted, with angiography – the absence of atherosclerosis. It can be difficult to exclude cardiac syndrome in osteochondrosis, and this requires a long study.
radicular syndrome

The clinical manifestation of this syndrome is associated with one of the eight pairs of spinal nerve roots that innervate the cervical part of the spinal column. Characterized by unilateral lesion of the body.
The syndrome is associated with a violation of nerve conduction: with pain, or, conversely, with semi-paralysis (paresis), paralysis and decreased sensitivity.
Conduction disturbance is characterized by the following symptoms:
The first or second roots – numbness or, conversely, pain in the occipital region;
The third pair of roots – numbness of the tongue and the area behind the ears, difficulty in chewing food, a feeling of fullness of the tongue;
the fourth pair – pain in the collarbone, hiccups, difficulty in swallowing, as in the case of tonsillitis;
Fifth pair – violations are felt in the shoulder area in the form of difficulty in moving the arms;
Sixth pair – discomfort in the shoulder blades and forearm;
Seventh pair – numbness in the hands and, in particular, the index and middle fingers;
The eighth pair – leads to difficulties in owning the ring fingers and little fingers on the hands.
In practice, single vertebrae are very rarely affected, more often several pairs of nerve roots are involved in the pathogenesis, so the syndromes are mixed and confuse the clinical picture. It is desirable for the patient to independently listen to his own body.
Treatment of osteochondrosis of the cervical spine
Depending on the stage of the pathology (remission or exacerbation), the form of the disease (acute or chronic), the severity of clinical manifestations (the presence or absence of pain), various methods of therapy are selected.
It can be:
Conservative treatment (drug and non-drug);
Surgical intervention;
Combinations of conservative and operative techniques.
Let us dwell on the classical methods of therapy. Knowledge and competent use of simple techniques, including physiotherapy exercises, massage and self-massage, greatly facilitates the well-being of a person experiencing neck pain with osteochondrosis. In the case of long-term degenerative processes, it is better to undergo an examination in a hospital or outpatient setting, and only after that apply treatment procedures.
If it is not possible to undergo an examination, then it is recommended to use sparing methods, for example, to perform exercises aimed at hydration – saturation of the interarticular space with fluids by improving blood supply in the neck and neck.
Exercise therapy for cervical osteochondrosis
Therapeutic gymnastics, when performed correctly, works wonders. Many methods have been proposed, but all of them are based on enhanced nutrition of cartilage and bone tissues. The principle of exercise therapy is to restore blood supply to the damaged area of the body.
It is forbidden during exercise therapy to strongly rotate and bend your head, only imitation of such movements is allowed. This method has proven to be effective despite its apparent simplicity.
The correct use of exercise therapy is the use of physical exercises without:
Long loads on the joints of the neck (one set of exercises is performed no more than 2 minutes);
Turns, tilts and rotations of the neck (such exercises exacerbate pathological processes in the joints and intervertebral discs).
[Video] Dr. Evdokimenko – Gymnastics for the neck, exercises for the treatment of cervical osteochondrosis:
Self-massage for cervical osteochondrosis performed while sitting in a comfortable position. Use the methods of stroking, circular rubbing in the neck or shoulders. It is advisable to combine the self-massage method with rubbing in various ointments that increase blood flow and relieve pain in the kneaded area.
[Video] Self-massage technique for cervical osteochondrosis:
Выполнение простых правил профилактики, ЛФК и массаж (в некоторых случаях) позволяет вести комфортную жизнь с остеохондрозом шейного отдела позвоночника даже в пожилом возрасте.









