Contents
A trophic ulcer on the legs is an open type wound located on the skin of the lower extremities and formed against the background of tissue rejection. Trophic ulcers are prone to long-term existence, do not heal for 6 weeks or more. The pathological process involves not only the epithelium, but also the tissues located under it. After healing of trophic ulcers, scars remain on the skin. Even despite the high level of development of modern medicine, the treatment of trophic ulcers to this day remains one of the most difficult tasks.
The most common trophic ulcers of the legs and feet. According to statistics, up to 2 million people suffer from this pathology in the world. About 70% of cases of ulcers are associated with certain disorders in the functioning of the venous-vascular bed. Ulcers never arise spontaneously, they are preceded by a rather long process of development of serious pathologies in the body. The identification and treatment of trophic ulcers is carried out by such a branch of medicine as phlebology.
Causes of trophic ulcers

The causes of trophic ulcers are diverse, among them the following factors can be noted:
Varicose veins. It is varicose veins that contribute to the deterioration of the outflow of blood, leading to its stagnation. As a result, fresh blood, rich in nutrients, is unable to carry them to the tissues of the lower extremities. The result of such starvation is the gradual destruction of cells. Initially, a superficial wound is formed, which gradually transforms into an ulcer. It is with varicose veins that this problem occurs in half of the cases;
Venous thrombosis is another common cause of trophic ulcers. They have the same mechanism of development as in varicose veins, only the result of stagnation of blood is a blood clot that blocks the lumen of the artery;
Atherosclerosis of the arteries of the lower extremities is characterized by the formation of fatty plaques on the inner walls, which, as they grow, are able to completely block the lumen of the vessels. As a result of malnutrition, pathological processes begin to develop in the tissues, which lead to the formation of ulcers;
Martorella syndrome, which develops against the background of already existing hypertension and can lead to the formation of shunts inside the veins and arteries. It also causes circulatory disorders and becomes a trigger in the formation of trophic ulcers;
Diabetes mellitus can also lead to the formation of deep non-healing wounds on the legs;
Some systemic diseases, for example, vasculitis, collagenoses, blood diseases, metabolic disorders, can become the cause of the development of this pathology;
If the rules of personal hygiene are not followed, pyoderma occurs, which can lead to the formation of ulcers;
Lyell’s toxic epidermal necrolysis is considered an etiological factor;
Any diseases of the cardiovascular system can provoke the development of trophic ulcers. They occur as a result of pronounced edema of the lower extremities against the background of circulatory failure;
Infectious diseases can lead to the formation of trophic ulcers – these are tuberculosis, syphilis, infectious tropical disease, Naga ulcer, onchocerciasis, leishmaniasis, etc .;
Trophic ulcers may be the result of malignancy of various skin formations or occur with radiation damage to the skin;
The provoking factors are burns and frostbite of the lower extremities.
According to available statistics, in 52% of cases trophic ulcers have a varicose etiology, in 14% of cases their occurrence is associated with impaired functioning of the arteries, in 13% trophic ulcers occur as a result of several factors. The share of ulcers resulting from vein thrombosis accounts for 7% of cases. Due to trauma, ulcers appear in 6% of cases. Diabetic ulcers account for 5% of the total number of diagnoses.
In general, any disease of the veins of the lower extremities (both deep and superficial) with venous insufficiency can lead to the formation of ulcers. At the same time, even minor scratches and wounds can cause a wound that does not heal for a long time.
Trophic ulcer in diabetes mellitus
A trophic ulcer in diabetes mellitus or a diabetic ulcer occurs as a complication of the underlying disease. It is known that in diabetes mellitus there is a violation of the absorption of glucose. The walls of the vessels become rigid, diabetic neuropathy and diabetic angiopathy are formed. In the affected areas, blood circulation becomes difficult, and the lack of tissue nutrition leads to the formation of ulcers.
The danger of a diabetic ulcer is that it can transform into gangrene, which will lead to the need for amputation of the limb.
Symptoms of trophic ulcers

Symptoms of trophic ulcers depend on what caused their formation:
Symptoms of venous trophic ulcers. The formation of a trophic ulcer of venous origin is always preceded by the occurrence of specific signs indicating the progression of damage to the venous system.
At the very beginning of the disease, people notice that they have increased swelling of the legs. There is a feeling of heaviness in the area of calves and shins.
At night, convulsions may appear, which tend to become more frequent. In parallel, there is a burning sensation and itching in the lower extremities.
Pigment accumulates in the skin, making the skin darker. As the disease progresses, the hyperpigmented area increases in size.
Hemosiderin accumulates in the skin, provoking the development of eczema and dermatitis. The skin itself thickens, acquires a lacquer sheen, and when touched, it responds with painful sensations.
Lymphostasis is growing, it can lead to the fact that lymph seeps out through the skin and appears on its surface in the form of dew drops.
As the disease progresses, a pre-ulcerative condition develops, when a white patch of epidermal atrophy appears in the center of the affected area. In this case, a person may not notice such minimal damage to the skin until an ulcerative defect appears in the atrophied zone. Initially, it has a small size, and the ulcer itself is located on the surface.
Over time, the ulcer begins to deepen, becoming larger in diameter. If several ulcers occur, they can merge, forming extensive lesions.
The pathological process tends to expand not only to the sides, but also to grow in depth. The deeper the ulcer penetrates, the more intense the pain becomes.
It is possible to involve the calf muscles, the Achilles tendon, the frontal surface of the tibia in the process. If the process has spread to the bone tissue, this can provoke the development of osteomyelitis.
The contents of a different nature are released from the ulcer. Initially, it is hemorrhagic, then becomes cloudy, may contain fibrin threads or pus. An unpleasant odor emanates from the wound. Often, microbial eczema forms around a trophic ulcer.
There is a risk of secondary infection, which can be triggered by opportunistic bacteria against the background of a decrease in local and general immunity. In the elderly, trophic ulcers are often complicated by mycotic infection. This greatly worsens the prognosis.
Trophic ulcers are accompanied by severe pain and cause unbearable suffering to a person.
Symptoms of a diabetic ulcer. A diabetic ulcer develops against the background of diabetes mellitus and is expressed in the following signs:
At the initial stage of development of a diabetic ulcer, there is a loss of sensation in the lower extremities. This is due to the death of nerve endings.
At night, a person begins to experience pain.
The place of localization of a diabetic ulcer is the big toes of the foot, or the tops of the phalanges of the fingers. On the sole, it can form in the place where the corns are located – this is the surface of the foot or heel.
As the disease progresses, a small but deep wound appears. Then it increases in size.
More often than other ulcers, a diabetic trophic ulcer is complicated by gangrene and leads to limb amputation.
Symptoms of atherosclerotic trophic ulcers. Atherosclerotic trophic ulcers are formed against the background of vascular atherosclerosis and have the following clinical picture:
For the initial stage of development of an atherosclerotic trophic ulcer, intermittent claudication is characteristic. The sensitivity of the diseased limb is disturbed, it gets tired faster, often freezes.
The place of localization of ulcers is the outer side of the foot, the phalanx of the big toe, the heel zone.
Ulcers are small, semicircular in shape.
The edges of the ulcer are denser, torn. The skin surrounding the edges of the ulcer has a yellowish tint.
The contents of the ulcer are purulent. As the disease progresses, the ulcers fill the entire surface of the foot.
Symptoms of trophic ulcers Martorella. This type of trophic ulcers is formed against the background of an increase in blood pressure. Most often, such ulcers affect women aged 40 years and older.
A characteristic feature of ulcers in Martorell’s syndrome is the formation of a papule on the lower limb, which responds with mild pain. As the disease progresses, the papule transforms into an ulcer.
Another distinguishing feature of hypertensive ulcers is the symmetry of their occurrence. That is, they occur on both limbs at once, most often in the central part of the lower leg.
Ulceration progresses slowly and is particularly painful. There is an increased risk of bacterial infection.
Stages of a trophic ulcer
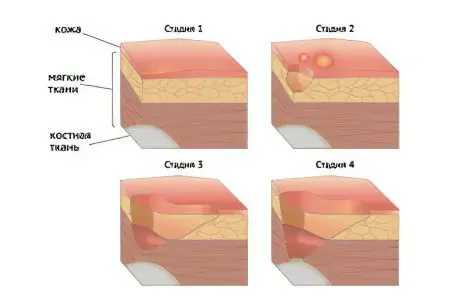
In the process of the development of the disease, four main stages of a trophic ulcer are distinguished, among which:
The stage of exudation (the beginning of inflammation, the appearance of necrotic foci);
Stage of repair (cleansing the surface of the ulcer from necrotic contents, the formation of granules, reducing inflammation);
Stage of epithelization (appearance of fresh epithelium, healing of the wound);
The stage of tissue scarring (the final stage, when scar tissue forms at the site of the existing ulcer).
The stages of trophic ulcers may differ slightly depending on what caused them. These differences are typical for the initial stage of inflammation, the stage of repair, epithelialization and scarring are all ulcers with an uncomplicated course of the disease.
Complications and consequences of trophic ulcers
The prolonged existence of a defect can cause conditions that are unfavorable to human health, which can lead to hospitalization.
Complications and consequences of trophic ulcers can be as follows:
Pyoderma;
microbial eczema;
allergic dermatitis;
fungal infection;
Lymphangitis, erysipelas, inguinal lymphadenitis;
Varicothrombophlebitis;
Phlegmon;
Gangrene;
Tetanus;
Arthritis, arthrosis, periostitis, tendinitis, osteomyelitis;
Wound malignancy (from 1,6 to 3,5% of cases);
Wound myiasis, that is, the colonization of the ulcer by insect larvae;
Development of bleeding;
Sepsis;
secondary lymphedema.
Answers to popular questions
Is a trophic ulcer on the leg contagious? No, a trophic ulcer on the leg is not contagious.
Is it possible to wet a trophic ulcer on the leg? Wetting a trophic ulcer on the leg is not recommended, as this can lead to the development of complications and the addition of a bacterial infection. It is necessary to treat the ulcer with the help of special antibacterial, antiseptic and drying agents.
Which doctor treats trophic ulcers? Trophic ulcers are treated by a phlebologist surgeon.
How and how to treat a trophic ulcer?
The specialist and the patient face a whole range of tasks. First, it is necessary to minimize the manifestations of the underlying disease, which led to the formation of an ulcer. That is, it is necessary to carry out therapy for varicose veins, lower blood pressure, treat diabetes. Secondly, it is necessary to carry out measures aimed at healing the trophic ulcer itself.
General conservative therapy is reduced to the use of the following means:
Treatment of the underlying disease with the use of phlebotonics, antiplatelet agents, antiplatelet agents. They allow you to adjust the processes of blood clotting, contribute to the normalization of blood circulation, prevent venous stasis;
Antibacterial therapy is selected taking into account the sensitivity of the microorganisms inhabiting the ulcer to specific antibiotics. It is possible to use preparations in the form of ointments or sprays for topical application;
To accelerate the processes of regeneration, drugs are prescribed that affect metabolic processes in tissues;
Painkillers are prescribed to relieve pain.
Hygiene of trophic ulcers should be regular. To begin with, the wound is washed with sterile saline, dead tissue and exudate are removed from it. After the sanitation, an antibacterial agent is applied and the ulcer is covered with a bandage. If the wound is at the healing stage, then the bandage should provide normal moisturizing and breathing of the wound surface. In the case where there is infection, a dressing should be chosen that can absorb secretions and provide an antiseptic effect. For this, special napkins are used.
It is possible to undergo physiotherapy procedures that help accelerate the healing of the ulcer. The following methods are effective: ultrasonic cavitation of the wound, UV irradiation, hyperbaric oxygen therapy, laser therapy, magnetotherapy.
When the ulcer heals and the patient feels well, surgery may be performed. It will be aimed at normalizing venous and arterial outflow, at removing veins that have undergone varicose expansion.
Treatment of trophic ulcers should be comprehensive and timely, an indispensable condition is getting rid of the underlying disease. This is the only way to avoid serious complications and prevent the recurrence of the disease.










MIMI NKO 6 IYA NAKIDODA WA MUGUU NA SIJUI IFAYANINI NA SIJUI NINI NITOKE KWAKITADANI