Contents
Inflammation of the gastric mucosa is one of the most common human diseases. Approximately 80-90% of people during their lives had at least one episode of this disease. In old age, up to 70-90% of people suffer from various forms of gastritis. The chronic form of gastritis can transform into peptic ulcer, stomach cancer.
What is gastritis?
Gastritis is an inflammation of the mucous layer of the stomach, leading to dysfunction of this organ. When gastritis occurs, food begins to be poorly digested, which results in a breakdown and lack of energy. Gastritis, like most diseases, is acute and chronic. In addition, there are gastritis with low, normal and high acidity of the stomach.
Currently, gastritis can already be called the disease of the century. They hurt both adults and children. And according to health statistics, in Russia about 50% of the population has gastritis in some form.
Gastritis is characterized by a variety of external and internal causes that provoke the development of pathology. Clinically, it occurs in the form of inflammation (acute or chronic). Acute inflammation is short lived. Damage to the mucous membranes of the stomach with concentrated acids, alkalis and other chemicals is dangerously fatal.
A long-term (chronic) flowing disease reduces the quality of life and manifests itself in the form of pain, as well as:
Heaviness in the abdomen;
heartburn;
Belching;
vomiting;
Diarrhea and/or constipation;
Bloating;
Flatulence – gas discharge;
Bad breath.
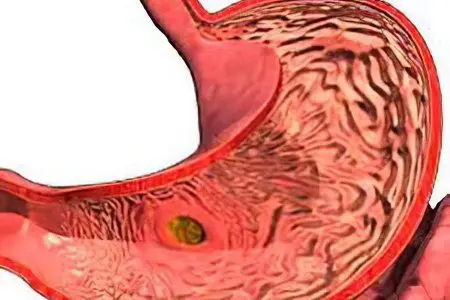
The chronic form is dangerous atrophy of the gastric mucosa. As a result, the glands of the stomach cease to function normally. Atypical cells are formed in place of healthy cells. An imbalance in the process of self-healing of the cells of the gastric mucosa is one of the causes of ulcers and cancer of the gastrointestinal tract.
The stomach is the most vulnerable section of the digestive system. At least three complex processes of digestion take place in it: this is the mechanical mixing of the food coma, the chemical breakdown of food, and the absorption of nutrients.
The inner wall of the stomach, the mucous membrane, is most often damaged, where two mutually exclusive components of digestion are produced – gastric juice and protective mucus.
Digestion in the stomach is a finely tuned biochemical process of the body. This is confirmed by the normal acidic pH of the gastric juice (its main component is hydrochloric acid), but also by the difference in acidity parameters in its different parts. High acidity (pH 1,0-1.2) is observed in the initial part of the stomach, and low (pH 5,0-6,0) – at the junction of the stomach with the small intestine.
The paradox lies in the fact that in a healthy person, the stomach not only does not digest itself, but also the gastric juice produced by the glands in different parts of the body has different properties. At the same time, the pH environment in the esophagus is neutral, and in the duodenum (the first section of the small intestine) it is alkaline.
An unpleasant, painful sensation of a person with gastritis – heartburn – is primarily the result of a violation of the acid-base balance in one of the sections of the gastrointestinal tract. In addition, the deviation of the acid balance from the norm in certain parts of the stomach underlies the pathogenesis of gastritis with low or high acidity.
A gross impact on the digestive process: food or chemical poisoning, the release of bile into the stomach, intestinal infections, regular intake of certain medications, carbonated drinks, alcohol and other factors negatively affect the condition of the gastric mucosa. The serious influence of the microbial factor on the development of gastritis has been proven.
A short-term emergency effect on the digestive process is limited to clinical manifestations in the form of acute inflammation of the following nature:

Catarrhal;
fibrinous;
Necrotic;
Phlegmonous.
Catarrhal gastritis is associated with poor nutrition and mild food poisoning. Fibrinous and necrotic gastritis is usually caused by poisoning with salts of heavy metals, concentrated acids and alkalis. Phlegmonous gastritis is caused by traumatic damage to the stomach wall.
Prolonged exposure to a weakened organism ends with the development of chronic pathogenesis, aggravated by ulcerative processes on the walls of the stomach. Gastritis can be harbingers of oncological processes in the gastrointestinal tract.
The variety of manifestations of gastritis of the stomach in humans is confirmed by their complex classification. Detailing the clinical symptoms of gastritis is essential for gastroenterologists when prescribing treatment procedures. In our case, this is an illustration of various forms of the disease in order to form a generalized idea of gastritis in the reader.
Another group of gastritis is not associated with microbes, although at certain stages this connection may appear.
Non-microbial gastritis are divided into several groups:
Alcoholic. The disease develops under the influence of regular use of strong alcoholic beverages (alcohol has an alkaline pH) against the background of numerous other factors associated with the general negative effect of large doses of ethyl alcohol on the body;
NSAID-induced gastritis. NSAIDs are non-steroidal anti-inflammatory drugs that are used in many diseases as antipyretic, analgesic and antiplatelet drugs. The most famous drugs of this pharmacological group are acetylsalicylic acid (aspirin), analgin, diclofenac, indomethacin, ketoprofen, ibuprofen, piroxicam. Uncontrolled use of NSAIDs stimulates the development of gastritis, and then its transformation into gastric ulcer.
Post-resection. Such gastritis develops after forced surgical removal of part of the stomach.
Chemically caused gastritis. They develop as a result of accidental or special ingestion of chemicals that have aggressive properties against proteins of the mucous membranes of the stomach.
Gastritis of unknown origin.
In professional medicine, other classifications of gastritis are also used, including, according to the type of spread of pathogenesis:
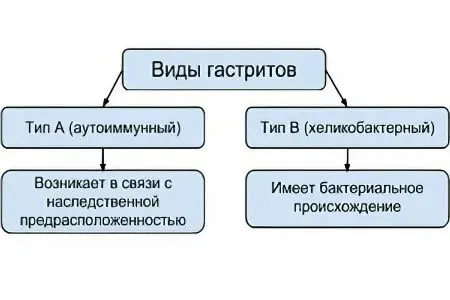
Autoimmune gastritis (type A);
Exogenous gastritis (type B), provoked by Helicobacter pylori;
Mixed gastritis (type A + B);
Gastritis (type C) provoked by NSAIDs, chemical irritants or bile;
Special forms of gastritis;
Gastritis against the background of a decrease and increase in the secretion of hydrochloric acid;
Other forms of morphological and functional manifestations of gastritis.
Their differentiation involves the use of complex medical laboratory or instrumental techniques at the stage of diagnosing the disease. Therefore, the description of gastritis, which have approximately the same clinical symptoms, but differ in the underlying mechanisms of pathogenesis, is not of interest to a wide range of readers.
Let us dwell in detail on the main signs and symptoms of gastritis, which can serve as a basis for a person to contact a medical institution for help.
Signs and symptoms of stomach gastritis
Gastritis is characterized by a variety of symptoms, but can occur without pronounced manifestations. The most characteristic symptom is pain in the solar plexus, which is aggravated after taking certain types of food, liquids and drugs, especially those that have increased aggressiveness to the gastric mucosa. Sometimes the pain gets worse between meals. With gastritis, spicy foods, alcohol, carbonated drinks and other foods, the use of which leads to an exacerbation of gastritis, are contraindicated.
Important, but less constant signs of gastritis are heartburn, vomiting, and belching. The disease is sometimes manifested by bloating and frequent gas discharge. The appearance of two or more of the above symptoms against the background of abdominal pain is a reason to suspect gastritis.
The disease is also indicated by the intake of spicy food, drugs and aggressive liquids shortly before the onset of pain.
It is much more difficult to identify the symptoms of chronic gastritis. For a long time, the signs of the disease are limited to irregular stools, plaque on the tongue, fatigue, rumbling and overflow in the abdomen between meals, flatulence, recurrent diarrhea or constipation.
Chronic gastritis usually does not have a significant impact on the patient’s clinical condition, with the exception of a decrease in the quality of life. In mild form, chronic gastritis is characterized by constipation and diarrhea. In severe form, except for those indicated – frequent discharge of intestinal gases, anemia, drowsiness, cold sweating, increased peristalsis, halitosis.
Symptoms of high acidity
The most common signs of gastritis with high acidity, in addition to general symptoms (vomiting, nausea):
Prolonged pain in the solar plexus, disappearing after eating;
Frequent diarrhea;
Heartburn after eating sour food;
Frequent urge to pass gases from the mouth – belching.
Symptoms of low acidity
The most common signs of gastritis with low or zero acidity:
Persistent bad taste in the mouth
Heaviness in the abdomen after eating;
“Burping” rotten eggs “;
Rumbling;
Nausea in the morning;
Problems with bowel regularity;
Disgusting odor from the mouth.
Symptoms of exacerbation of gastritis

The recurrence of chronic gastritis is characterized by a variety of symptoms, the most common symptoms are:
Constant or periodic pain in the solar plexus, which increases immediately after eating, or vice versa, with prolonged fasting;
Belching with air, burning in the sternum, heartburn after eating, metallic taste in the mouth;
Nausea, morning vomiting of semi-digested food with a characteristic sour taste, sometimes vomiting of bile;
Increased salivation, thirst, weakness;
Manifestations of dyspepsia (constipation, diarrhea);
Dizziness, palpitations, headache.
Symptoms of exacerbation of erosive (severe) forms of gastritis are supplemented by vomiting with blood clots, sometimes vomiting with a dark color of vomit. Gastric bleeding during bowel movements is manifested by black feces. Sometimes gastric bleeding can only be determined by laboratory methods. Massive internal bleeding is manifested by pallor of the skin and mucous membranes and is easily determined by the color of the sclera of the eyes, dizziness, and tinnitus.
Pain in the stomach with gastritis
Gastralgia – pain in the abdominal wall (cavity) – an important symptom of gastritis. Meanwhile, pains are accompanied by other diseases of the abdominal organs, which are collectively called “acute abdomen”. Unpleasant sensations are manifested in the form of pain, as well as stabbing, pressing, shooting, burning and other types of pain.
Pain resembling gastralgia can be a symptom of myocardial infarction, inflammation of the membranes of the heart and lungs, and rib fractures. Pain in the stomach can be observed with viral, bacterial and parasitic pathologies in the intestines, specific women’s problems, neurosis, diabetes.
At home, you can recognize the pain caused precisely by gastritis. The most characteristic of gastritis and distinguishing it from other pathologies of the “acute abdomen” are pains that increase after:
Eating, especially spicy and smoked;
Use of alcohol or certain medications, in particular non-steroidal anti-inflammatory drugs;
Prolonged break from eating.
The remaining options for the occurrence of pain in the stomach in the absence of clinical skills and the ability to use laboratory and instrumental research methods can be easily confused with symptoms of other ailments.
Causes of gastritis
Of greatest interest are the causes that cause the chronic form of gastritis. Allocate external and internal factors that provoke the development of the disease. Interestingly, in some people, gastritis develops much more slowly and does not have a significant effect on the body. That is, most likely, the causes of gastritis are hidden behind many factors and their combinations.
The most significant external causes of gastritis:
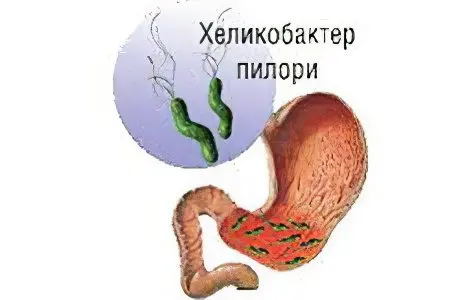
Impact on the walls of the stomach of bacteria Helicobacter pylori, less often other bacteria and fungi. Approximately 80% of patients diagnosed with gastritis secrete acid-resistant bacteria that actively penetrate into the wall of the gastric mucosa, secrete specific substances that irritate the mucous membrane, stimulate a local change in the pH of the walls and their inflammation. The final answer, why these bacteria cause significant harm to some people, and not to others, is still unknown;
Eating disorders. It has been established that poor nutrition is a common cause of gastritis. The statement is true for both overeating and undereating. It is necessary to diversify the diet with plant foods rich in vitamins and plant fiber, which normalizes peristalsis. However, with the development of the initial stages of gastritis, it is necessary to avoid foods containing coarse vegetable fiber, as well as fatty, spicy, canned and pickled foods;
Alcohol abuse is isolated as a separate cause of gastritis of the stomach. Ethanol in small amounts is an important component of the biochemical processes in the body, however, a large amount of alcohol provokes an acid-base imbalance in the body. In addition, alcohol in large doses with regular use significantly harms other digestive organs – the liver, pancreas, and also has a detrimental effect on metabolic processes in the body;
It has been noted that some drugs widely used in medicine as anti-clotting (antiplatelet), analgesic and anti-inflammatory drugs have a serious side effect – they irritate the gastric mucosa. Most often, gastritis is caused by non-hormonal anti-inflammatory drugs (aspirin, analgin) and glucocorticoid hormones (prednisone). These medicines are recommended to be used strictly for medical purposes, fractionally, in small doses, after meals;
Some researchers note the impact on the development of gastritis of helminthic invasions, chronic stress, aggressive chemicals, swallowed accidentally or intentionally.
The main internal (related to the violation of homeostasis) causes of gastritis:
Congenital human predisposition to gastrointestinal diseases;
Duodenal reflux – pathological throwing of bile from the duodenum into the stomach. Bile, getting into the cavity of the stomach, changes the pH of the juice and irritates the mucous membrane. Initially, inflammation of the antrum of the stomach develops, and then its other departments are involved;
Autoimmune processes, damage at the immune level of the protective properties of the cells of the gastric mucosa. As a result, the cells stop functioning normally and lose their original properties. This phenomenon triggers a cascade of small reactions that change the pH of the juice, and leads to constant irritation of the stomach walls. There is endogenous intoxication and a violation of the resistance of the mucous membrane to the aggressive environment of gastric juice;
Violations of hormonal and vitamin metabolism, the reflex effect of the pathogenesis of organs adjacent to the stomach.
Types of gastritis:
With the help of instrumental and functional methods, many variants of gastritis were diagnosed. However, everyone is divided into gastritis with:
Normal or increased acidity;
Zero or low acidity.
Symptoms of gastritis with low or high acidity can generally be distinguished, however, the final diagnosis is made on the basis of a study of gastric juice obtained by probing, as well as intragastric pH-metry using special sensors inserted into the stomach. The latter method is convenient in that long-term monitoring of gastric juice parameters is possible. In some cases, the pH of gastric contents is determined indirectly, in the study of urine pH.
Acidic gastritis
It is characterized by severe pain in the solar plexus or in the navel, usually of a paroxysmal nature. The pain subsides after taking dietary food, intensifies in between meals. Pain in the right hypochondrium is evidence of the ingress of gastric juice into the duodenum. Pathology is characterized by heartburn, morning sickness, rotten belching, rumbling in the abdomen, diarrhea (constipation is more common for gastritis with low acidity), a taste of metal in the mouth.
In some cases, the disease proceeds subclinically, with periodic exacerbations after drinking alcohol, drugs of the NSAID group, cardiac glycosides (digitis), potassium preparations, hormones (prednisolone, dexamethasone, hydrocortisone). The attack can be provoked by the use of “heavy” food. The type of gastritis is determined by medical research.
Gastritis with low acidity
The acid in the stomach is involved in the primary breakdown of coarse food fibers.
Gastritis with low acidity is more often manifested by heaviness in the abdomen, rapid satiety after eating, increased formation of intestinal gases. In some cases, the disease can be corrected by taking digestive enzymes (festal, gastal). You can treat anacid gastritis at home, it’s very simple. Since gastric juice has reduced properties, you should chew food for a long time. Careful grinding of the food coma in the oral cavity and processing it with saliva is an effective non-medical method of treating gastritis.
Acute gastritis

Catarrhal gastritis develops under the influence of aggressive drugs (aspirin, other NSAIDs), harmful drinks (alcohol, carbonated lemonades with frequent use) and heavy foods (fatty, salty, smoked, pickled). Acute gastritis is also known against the background of toxic infections (salmonellosis and others), as well as against the background of renal and liver failure. Acute forms of gastritis can be provoked by pathologies not directly related to the gastrointestinal tract (pneumonia, frostbite). This is due to the accumulation of underoxidized products in the blood during severe inflammation of the lungs, which causes inflammation of the walls of the stomach. Describe also acute gastritis on the background of stress.
Phlegmonous gastritis – a consequence of intentional or accidental injury to the walls of the stomach (swallowed pins, glass, nails). The disease is manifested by purulent fusion of the walls of the stomach.
Symptoms of catarrhal (simple) acute gastritis appear 5-8 hours after exposure to a crisis factor. Pathogenesis begins with a burning sensation in the epigastric region (synonyms: in the pit of the stomach, in the solar plexus). Pain develops in this area, nausea, vomiting, metallic taste in the mouth. Toxic-infectious gastritis is supplemented by fever, persistent vomiting and diarrhea. A severe condition is characterized by bloody vomiting – this is a corrosive (necrotic) gastritis. Phlegmonous gastritis is manifested by the phenomena of peritonitis: a tense abdominal wall, a state of shock.
Chronic gastritis
In the initial stages, the disease proceeds without bright symptoms. Hypersensitivity to certain types of food is periodically manifested in the form of heartburn and bloating. Often there is a feeling of heaviness with a full stomach, a plaque and a peculiar pattern are found on the tongue.
The chronic form of gastritis can develop at any age: from 20 years to old age. The disease is characterized by periods of exacerbation and remission. During the period of exacerbation, the signs of chronic gastritis do not differ from the symptoms of the acute form of the disease – pain, combined with nausea, sometimes vomiting. Unpleasant sensations are aggravated after taking certain types of food. Usually this is a certain set of products that you should remember and try to exclude from the diet or limit consumption.
Pallor of the mucous membranes may be a sign of another disease – atrophic gastritis. It occurs on the background of a deficiency in the body of vitamin B12. This vitamin is very important for blood formation. Atrophic gastritis may not have other striking signs, except for pallor. The danger of the disease is that it is a harbinger of the development of cancer cells in the epithelium of the stomach. The detection of anemia against the background of signs of gastritis is an occasion to more closely examine the state of health.
The human body has large-scale protective resources, so lifestyle changes, dietary intake and properly prescribed complex treatment significantly increase the likelihood of a cure for any form of gastritis.
How can you help yourself at home?

A common cause of gastritis is the excessive consumption of the following two substances:
Aspirin (acetylsalicylic acid);
Alcohol (ethyl alcohol, ethanol).
Aspirin and its analogues are prescribed by cardiologists for long-term daily and mandatory use in order to prevent myocardial infarctions and strokes. Tens of thousands of people daily take aspirin as a means of inhibiting the formation of blood clots, which makes the problem of the safe use of NSAIDs very urgent.
Acetylsalicylic acid preparations have excellent antiplatelet properties, that is, they prevent the development of blood clots in the vessels. Blood clots are the main cause of myocardial infarction and cerebral stroke. However, aspirin and other NSAIDs have an unpleasant side effect – they irritate the mucous membranes of the gastrointestinal tract. Hypertensive patients use these drugs daily in combination with other drugs. Immoderate intake of aspirin and its analogues can provoke an additional problem for a sick person – gastritis. This is true for all people of the older age group suffering from hypertension, angina pectoris, who have suffered or are at risk of developing myocardial infarction.
Alcoholwidely used by certain categories of citizens. In people predisposed to diseases of the gastrointestinal tract, even moderate consumption of ethanol can provoke an exacerbation of gastritis. Alcohol has alkaline properties. Regular neutralization of the acidic environment of the stomach with ethanol creates a condition for irritation of the walls.
Meanwhile, there is no reason to exclude aspirin and other important drugs (iron, potassium, hormones, etc.) from the list of useful medicines. Carefully read the annotations to the medicines and take them according to the scheme recommended by the doctor.
In particular, you can reduce the side effects of taking aspirin in the following ways:
Reduced single dose (consult your doctor);
Taking the drug on the eve of a meal;
Drinking large volumes of water;
The transition from aspirin to modern shell analogues (THROMBO-ASS).
When prescribing aspirin and other NSAIDs, caution should be exercised if the patient has:
Erosive and peptic ulcer disease in the acute stage;
Individual intolerance to acetylsalicylic acid preparations;
Tendency to gastrointestinal bleeding;
Bronchial asthma;
kidney failure;
Pregnancy in women.
Always tell your doctor if you have any restrictions on the use of aspirin. This will help the doctor to navigate, choose the correct dosage of the drug, replace it with more suitable analogues or drugs of a different pharmacological group, adjust the methods of application, and reduce the frequency of aspirin use.
The irrational use of any drugs can have negative consequences and impede the absorption of other prescribed drugs. Antacids containing aluminum in large doses cause constipation, potassium-containing medicines reduce the acidity of the stomach (in some cases this is a useful property). Potassium is also beneficial for women during menopause.
In case of intolerance to certain groups of drugs, they are replaced by others. For example, histamine-H2 blockers can be such substitutes. Drugs in this group (cimetidine, ranitidine) are over-the-counter drugs. These tablets are prescribed as a means of regulating acidity in the stomach, and, as a result, reducing pain in hyperacid gastritis.
As for alcohol, it should be abandoned during the period of exacerbation of gastritis and the use of pharmacological agents that have an aggressive effect on the gastrointestinal tract. Regular alcohol consumption is a real threat to the development of gastritis of the stomach.
Medicines for gastritis of the stomach
In the arsenal of gastroenterologists for the treatment and prevention of gastritis, there are several pharmacological groups of drugs, including:
Enterosorbents – activated carbon, smecta;
Antacids;
Antiseptics and disinfectants;
antidiarrheal drugs;
Tetracycline antibiotics;
Antihistamines (H2 subtype).









