Contents
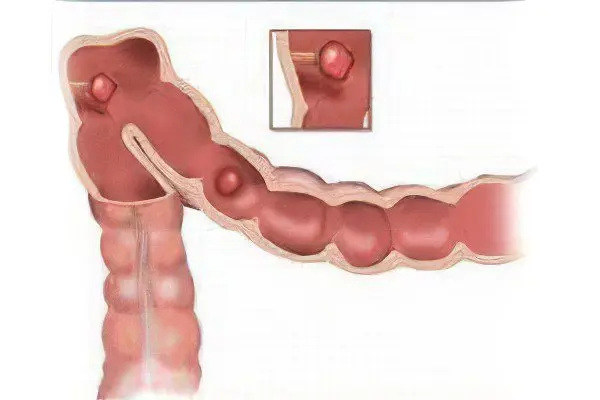
Polyps in the intestines are benign neoplasms, often localized on its inner walls, as in other hollow organs. Such outgrowths are formed from the glandular epithelium and protrude into the lumen of the intestines, sometimes they are held on a stalk, and sometimes it is absent, and then they talk about polyps on a wide base.
Intestinal polyps are classified as precancerous diseases, as they often undergo malignant transformation (especially in the hereditary form of polyposis). Therefore, when they are found in the intestines, doctors unambiguously recommend surgical removal. The difficulty in diagnosing the disease lies in the fact that polyps give mild symptoms, although sometimes it is possible to suspect their presence by a number of clinical signs (bloating, constipation, itching, and sensation of a foreign body in the anus).
The consistency of the formations is soft, as for the shape, it can be varied: spherical, branched, mushroom-shaped. Most often, growths form in the rectum or in the lower colon. In the higher sections of the intestine, polyps are extremely rare. For example, only in 0,15% of cases they are detected in the duodenum. Their color varies, it can be dark red, reddish gray, with a yellow tint. Sometimes mucus is found on the surface of the polyps.
According to statistics, intestinal polyposis is a common disease. About 10% of people over the age of 40 have benign tumors in the intestines. Moreover, in men they are formed 1,5 times more often. The sooner the pathology is detected, the higher the chances of preventing its malignancy. Often this helps to make a study of fecal masses for occult blood. When an operation to remove polyps from the intestines is carried out in a timely manner, in 90% of cases it becomes the key to a person’s survival.
Symptoms of polyps in the intestine
It is often impossible to suspect the presence of a polyp by certain symptoms, due to the absence of specific clinical manifestations of the pathology. The degree of their severity depends on the size of the formation, where exactly in the intestine they are located, and also on whether their malignancy has occurred or not.
Among the possible symptoms of polyps in the intestines:
The secretion of mucus and blood, which is most often observed in the presence of villous adenomas;
If the polyps are of impressive size, then the patient complains of recurrent pains that have a cramping character. They occur in the lower abdomen. In addition, mucus and blood are observed, as well as constipation occurring in the form of intestinal obstruction. Often with large polyps, a person experiences a sensation of a foreign body in the anus;
In parallel with polyps, the patient often has other pathologies of the digestive tract, which force him to undergo a complete examination, during which a neoplasm is accidentally detected;
The development of colorectal cancer occurs 5-15 years after the formation of a villous adenomatous polyp. Malignancy occurs in 90% of cases;
Obvious symptoms of polyps are permanent violations of peristalsis. It can be diarrhea and constipation. The larger the formation, the more often constipation occurs, as the intestinal lumen narrows. As a result, partial intestinal obstruction is formed;
The patient may experience a feeling of fullness in the stomach, suffer from belching and nausea;
With the appearance of pain in the intestinal area, one can suspect the onset of an inflammatory process;
An emergency reason for contacting a doctor is the onset of bleeding from the anus. This is a fairly serious symptom and may indicate a malignant process in the intestine;
If the polyp has a long stalk, then it can protrude from the anus, although this is quite rare;
Hypokalemia is the result of a malfunction of the intestine due to the presence of large polyps with finger-shaped processes in it. They secrete a significant amount of salts and water, thereby stimulating profuse diarrhea. This leads to a drop in the level of potassium in the blood.
Causes of polyps in the intestines

Modern medicine does not have unambiguous data on the etiology of intestinal polyposis.
However, there are certain theories that suggest a mechanism for the development of the disease:
Chronic inflammation of the intestinal wall. It has been established that polyps cannot begin to form in healthy tissues. Therefore, such an assumption regarding the cause of their occurrence seems to be the most obvious. Inflammatory processes occurring in the mucous membrane cause the epithelium to regenerate faster, and this can result in uncontrolled growth. In addition, scientists point to a link between the formation of intestinal polyps and diseases such as dysentery, ulcerative colitis, typhoid fever, enteritis, proctosigmoiditis. The basis for this hypothesis is the disappearance of relapses of polyposis after getting rid of these diseases. In addition, constipation and intestinal dyskinesia are capable of provoking the growth of polyps. It turned out that polyposis growths are more often found in the place of the intestine where there was stagnation of feces and there were microtraumas;
Global health problems for the majority of the population associated with environmental degradation. It is quite difficult not to notice the weakening of health in modern people. First of all, this applies to children. The number of babies with severe congenital pathologies is constantly increasing. Many children suffer from diseases that were previously characteristic of people only in extreme old age. The process of formation of polyps is also influenced by such factors as eating foods with chemicals, physical inactivity, lack of fresh air in living conditions in the city, alcohol abuse, smoking, eating disorders;
Pathologies of the digestive system and blood vessels. The condition of the intestinal mucosa largely depends on the blood vessels. Varicose and diverticular disease, atherosclerosis have a negative effect. Pathologies of the digestive system (stomach ulcer, gastritis, pancreatitis, cholecystitis and others) cannot but affect the health of the intestines;
Genetics. It is believed that burdened heredity has an impact on the development of the disease. This is confirmed by the fact that even against the background of absolute health, polyposis growths are found in some children. Scientists explain this fact by a genetic program that makes some sections of the intestine work differently;
embryonic theory. Scientists hypothesize that those areas of the intestine in which the formation of polyps occurs were incorrectly formed during prenatal development. Symptoms of the disease begin to appear somewhat later as a result of the influence of additional negative factors;
Food allergy, gluten intolerance. While just a few decades ago, gluten intolerance was a rare problem, now more and more children suffer from this form of food allergy. When products containing this protein enter the body, the immune system begins to react violently to it. She perceives gluten as a foreign agent, which leads to damage to the mucous membrane lining the intestines. If an inadequate immune response is ignored, a person is threatened with serious health problems, up to intestinal cancer and the development of osteoporosis.
In addition to the fact that there are common causes for the development of polyps in the intestine, the most likely factors for their formation in various departments have been put forward, for example:
Rarely forming polyposis growths inside the duodenum most often become the result of gastritis with high acidity, cholecystitis or cholelithiasis. The age of the diseased varies in the range from 30 to 60 years;
Even more rarely, formations are detected in the cavity of the small intestine. At the same time, they are combined with polyps in other parts of the intestine and in the stomach, and are more often diagnosed in women aged 20 to 60 years. The appearance of growths can be triggered by multiple factors, among which the inflammatory process is in the lead;
The formations found in the colon are most often the result of negative heredity.
What is the probability of polyp degeneration into colon cancer?
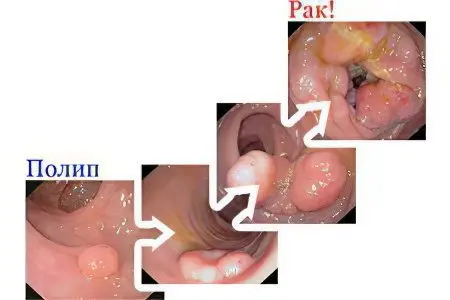
About 75% of all polyposis formations found in the intestine have the ability to malignancy. Such growths are called adenomatous. In order to determine the subtype of an adenomatous polyp, it is necessary to examine it under a microscope. Polyps can be tubular, glandular-villous, or simply villous. The most favorable prognosis in terms of malignancy is given by tubular formations. Villous polyps are the most dangerous and most often degenerate into cancer.
The size of the formation additionally affects whether the polyp is threatened with malignancy. The larger it is, the higher the risk. When the growth in volume exceeds 20 mm, the threat is aggravated by 20%. Due to the fact that even the smallest polyps will steadily increase, they must be removed immediately after detection.
There are also such varieties of polyps that are not threatened by malignancy – these are hyperplastic, inflammatory and hamartoma formations.
Adenomatous formations are the most dangerous. They have a high potential for malignancy.
Large polyps malignantly degenerate with a greater degree of probability.
Mandatory regular diagnostics
Colonoscopy, sigmoidoscopy and sigmoidoscopy are diagnostic procedures that are mandatory for regular passage for people over 50 years of age who have a dangerous heredity. If the growths are not detected, then the next time it is recommended to come to the clinic in two years;
After elimination of adenomatous formation, a person is shown a regular examination to identify new polyps in the intestine;
Modern medicine has special tests to diagnose a hereditary predisposition to the development of bowel cancer. This technique makes it possible to timely prevent the oncological degeneration of polyps.
Diagnostics
The early stage of the disease does not give bright symptoms, so most developed countries have introduced a mandatory annual stool test to detect occult blood in it. This analysis allows you to detect even invisible blood particles that come out with feces during bowel movements. However, even a negative test result cannot indicate that there is definitely no polyp in the intestine.
Techniques such as MRI and CT can detect growths in some parts of the intestine. To diagnose them in the rectum and sigmoid colon, it is more expedient to undergo sigmoidoscopy using a proctoscope. This device makes it possible to visualize the walls of the intestine in more detail. In addition, proctologists recommend prophylactic sigmoidoscopy every 5 years. This is a must for all people over 50 years of age.
Finger examination is another way to detect polyposis growths, fissures, tumors, cysts and hemorrhoids in the terminal rectum and in the anus.
Irrigoscopy allows visualization of formations larger than 10 mm. It is performed by injecting a contrast agent into the large intestine and taking x-rays.
However, the most modern and informative method for diagnosing polyposis is colonoscopy. It makes it possible to obtain information about any pathologies of the intestine, and if a polyp is found, you can immediately biopsy it. The resulting biopsy is sent for histological and cytological examination.
It is important for the doctor not to mistake the polyp for another, similar education:
Angioma. This is a tumor that has multiple vessels and is often manifested by severe bleeding;
Lipoma is a small tumor, often choosing the place of localization of the right side of the colon;
Myoma, provoking intestinal obstruction, is diagnosed quite rarely;
Non-epithelial tumor, which does not have a leg and at the same time reaches an impressive size;
Crohn’s disease can provoke pseudopolyposis, which is found in the upper part of the large intestine;
Actinomycosisaffecting the caecum.
Histology helps to differentiate the type of formation.
Popular questions and answers
Do colon polyps need to be removed? The answer to this question is unambiguously positive. Any polyp is subject to removal, its other treatment is impossible.
Does the stomach hurt with polyps in the intestines? Pain of a cramping nature can be observed with large polyps. At the same time, the lower abdomen and iliac region hurt. In addition, abdominal pain may appear against the background of inflammation that has joined.
Are intestinal polyps removed during rectoscopy? During this diagnostic study, small formations that are well located can be removed. In all other situations, surgical intervention is required.
Treatment of polyps in the intestine
After the polyp has been accurately differentiated, the doctor decides on the method of removal. As for drug treatment, it is not practiced, since it is not able to save the patient from growths. In some cases, medication is indicated, but this measure is temporary and allows you to prepare the patient for the upcoming operation. This is especially true for patients with a weakened immune system and in the elderly.
To reduce bloating, drugs from the group of antiflatulents, for example, Simethicone, are prescribed. In the presence of severe pain, it is recommended to take antispasmodics, for example, No-shpy.
Removal of polyps in the intestine

Regardless of the size of the formations, each of them must be removed. After this procedure, a microscopic examination is carried out for the presence of atypical cells.
The most popular ways to remove growths in the intestines are:
transrectal polyp excision
The procedure is performed with scissors or a scalpel. In this way, only polyps close to the anus can be removed from the body. They should be no further than 10 cm from the beginning of the anus, although a distance of 6 cm is considered optimal for such an operation.
The patient is given a local anesthetic. Most often, Novocain 0,25% is used for this. General anesthesia is rarely used. After the onset of anesthesia, the doctor, using a special mirror, pushes the anal canal apart and removes the polyp.
When the formation has a stalk, a Billroth clamp is used, with which the stalk is clamped. The defect formed on the mucous membrane is subject to suturing. For this, a maximum of 3 knots made with a catgut suture is sufficient. It does not require removal and completely resolves after a month. If the polyp is attached on a wide base, then the removal is performed by cutting out the neoplasm from the zone of a healthy mucous membrane using an oval incision.
In the case when the growths are located further than 6 cm, but closer than 10 cm from the entrance to the anus, the technology of the operation is somewhat modified. With the help of a rectal mirror, the anal canal is opened and further stretched with fingers until it is completely relaxed. Then a larger speculum is inserted, allowing the intestinal wall to be retracted without a polyp. Then a short mirror is inserted, and the patient needs to push. This allows the formation to be brought closer and gives the clinician the opportunity to capture it with an elongated Billroth forceps or fenestrated forceps. The doctor removes the short mirror, introduces additional anesthesia at the base of the polyp, and then removes it.
Endoscopic polypectomy
This method of removing a polyp is advisable to use if the formations are located in the middle (proximal) sections of the intestine. Such surgery is referred to as minimally invasive surgical methods that can be used in a state of drug-induced sleep of the patient. During the procedure, an endoscope is inserted into the anus, with which the polyp is found. After its detection, the neoplasm is removed using endoscopic instruments. Then the doctor makes sure that there is no bleeding and, if necessary, performs repeated coagulation. The polyp is removed from the patient’s body using an endoscope.
If the outgrowth is large, then it must be removed not entirely, but in parts. This procedure is called lumping. This is a rather complicated technique, during which an explosion of intestinal gases can occur, as well as perforation of the intestinal wall if the burn is too severe. Therefore, only a specially trained proctologist or endoscopist can perform such an operation. After removal of a large polyp exceeding 20 mm, the patient needs a second endoscopy after a year. A person is not removed from the register of a proctologist and every 3 years must undergo this procedure aimed at identifying a possible relapse of the disease.
Electroexcision
A rectoscope is inserted into the rectal cavity. An electric loop is carried out along it to the polyp. She pounces on the polyp, a current passes through it. The temperature of the loop rises, the epithelial tissue heats up. As a result, the tumor receives a thermal burn and dies. When the loop is tightened, the formation is cut off and brought out.
This method has a number of advantages, first of all, it allows you to prevent the development of bleeding, as there is an instant coagulation of the vessels.
Colotomy or bowel resection
The operation is indicated for the detection of polyps in the sigmoid colon, as well as for the diagnosis of fleecy formations with a wide base. The procedure will require general anesthesia. Then the doctor makes an incision in the left iliac region and the intestine is removed into the resulting lumen. The polypous area is palpated and opened. Previously, restrictive soft pulps are applied to healthy zones. The tumor and the part of the mucous membrane on which it is located are excised, then sutures are applied to this place. The intestine itself is sutured in two rows, and the anterior abdominal wall in layers.
Enterotomy
Surgical intervention aimed at removing polyps that are small and attached to the leg. Depending on which part of the intestine has undergone pathological growth, duodenotomy (duodenum), ileotomy (ileum), jejunotomy (jejunum) are distinguished. The necessary part of the small intestine is dissected with a scalpel or electric knife, the polyp is removed, and the resulting hole is sutured. The operation most often does not lead to complications, since the lumen narrows slightly with a standard enterotomy.
Segmental resection of the small intestine
The operation is indicated when large polyps are found in the small intestine, or if their base is wide. The entire area in which the growth is localized is excised. The ends of the intestine come together, and an inter-intestinal anastomosis is formed. Often such an intervention becomes the cause of digestive disorders in the future, as the patient suffers from “short bowel syndrome”.
As for the prognosis for recovery, it is favorable if the formation was detected at an early stage and promptly eliminated from the body. The longer the polyps are in the intestine and the larger their size and number, the higher the risk that they will degenerate into a malignant tumor. The probability of recurrence remains quite high even after complete removal of the tumor, it is up to 30%. Therefore, the follow-up of the patient and the passage of regular examinations are so important.
Diet after removal of polyps in the intestine

Rehabilitation of the patient after the operation primarily depends on the diet. Recovery consists of several stages and must take place according to certain rules.
After the operation, the first stage of the diet begins. It lasts for 3 days after the intervention. The patient is not allowed to drink or eat during the first 24 hours. When this time expires, a person can quench his thirst. The maximum volume of liquid taken at one time should not exceed 50 ml. In addition, the patient can drink vegetable broth, or compote based on unsweetened fruits. After another 12 hours, rice water, weak meat broth or jelly are allowed. You can also diversify the strict menu of the patient after the operation with a decoction of wild rose. Such restrictions are due to the fact that it is necessary to eliminate intestinal motility as much as possible and reduce its excretory function. The produced bile and digestive enzymes can adversely affect the condition of the seams and damaged tissues.
The second stage of the diet starts after three days after the intervention. If the patient feels satisfactory, then his diet can be expanded with the introduction of liquid cereals, meat soufflé (from lean meat), mucous soups and soft-boiled eggs. As for cereals, preference should be given to millet, oatmeal and rice. When a new product is introduced, it is necessary to carefully monitor the well-being of the patient. If, after eating a particular dish, there is an increase in gas formation, or painful sensations appear, then it is important to refuse such food. The second stage of the diet is aimed at consistently increasing the load on the operated intestine. At this time, the patient needs to normalize the stool. To adhere to such a diet should be until the moment of discharge from the hospital.
The third stage occurs two weeks after the operation. Over the next four months, the patient will have to adhere to a sparing diet.
The doctor should familiarize the patient with the basic rules of nutrition:
It’s important to stick to the routine. If the products will enter the body at the same time, this will allow the enzymes to begin to be produced in advance. In this case, the process of digestion will not be so difficult for the recovering intestine;
Small meals are needed. This will improve the motor function of the intestine, reduce the load on it. The number of meals should not be less than 6, but portions should be consumed small;
It is important to prevent fermentation processes in the intestines, as they can cause the development of peritonitis. For this, it is worth refusing to include legumes in the diet. The restriction includes nuts, asparagus and mushrooms;
To prevent constipation, the patient should receive a sufficient amount of fluid. Its volume depends on the patient’s body weight and averages 3 liters. Be sure to include first courses on the menu;
The fatter the food, the more bile is secreted. Its excess content negatively affects the process of regeneration of intestinal tissues;
It is important to stop eating too rough food that can injure the intestines. Products must be either thoroughly boiled or baked;
It is worth adding dairy products, eggs and lean meat to the diet. All of them contain protein, which contributes to the speedy recovery of tissues;
Sour, spicy and fried foods fall under a complete ban. This is due to their ability to chemically irritate the intestines.
The menu should be designed and compiled in such a way that it fully meets the needs of a person on the mend. This is important to do despite the existing limitations. Normal intestinal motility is the key to regular stools. This contributes to the prevention of dysbacteriosis and constipation, and therefore, to some extent, reduces the risk of re-formation of polyps.









