Contents
Myositis is an inflammation of one or more skeletal muscles. The disease differs in etiology, symptoms, nature of the course and localization. Inflammation, as it progresses, can spread to the heart, joints, intestines, skin, and lungs.
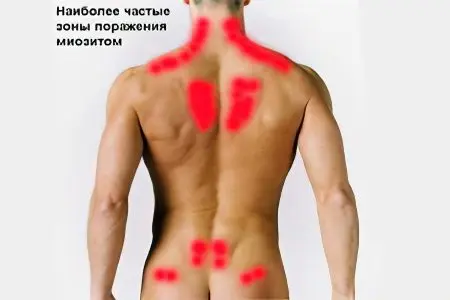
The disease is quite rare, so out of 1 million people, only one will suffer from myositis. But these statistics apply to those cases when myositis manifests itself as a systemic disease, that is, all skeletal muscles are involved in the inflammation process. The most common form of myositis is cervical myositis, it accounts for up to 60% of all cases of inflammation, the second most common form is lumbar myositis. It is believed that every person will encounter such varieties of the disease at least once in a lifetime.
Myositis can affect both adults and children, but dermatomyositis is more commonly diagnosed in childhood. Dermatomyositis in most cases affects the age group ranging from 1 to 15 years, although it can be found in adulthood. With regard to gender differences, women are more affected by dermatomyositis and polymyositis than men. After the age of 50, people are more likely to be diagnosed with fibromyositis.
Currently, myositis is called “office disease”, that is, the risk of its development increases with sedentary work. Some myositis may be a consequence of the profession, for example, inflammation of certain muscle groups in pianists and violinists.
Myositis can manifest itself as an independent disease or be a consequence of other diseases, it can be mild and disappear on its own after a few weeks, or it can be severe and disturb a person throughout life.
Causes of myositis
The causes of myositis may be due to the influence of exogenous and endogenous factors, including:
Infectious diseases. It is infections of a viral nature that are the most common causes of the development of myositis, less often inflammation of the muscles is provoked by bacterial agents. In this case, the infection from the base focus (for example, from the tonsils) spreads through the bloodstream to the muscle tissue. For influenza, SARS and other respiratory diseases, as well as for syphilis, tuberculosis, typhoid, non-purulent myositis is characteristic. Purulent myositis develops due to a generalized purulent infection, most often provoked by staphylococci and streptococci, osteomyelitis, or fungal microorganisms. In this case, myositis is severe and requires surgical treatment. It is also possible that muscles are directly affected by microorganisms, when inflammation develops due to the action of toxins on them, as waste products of pathogenic agents.
Autoimmune diseases. Most systemic diseases, especially collagenoses, are accompanied by myositis. The body, starting to produce antibodies against its own tissues, provokes muscle inflammation. Such myositis has either a subacute or chronic course and is accompanied by severe pain. Myositis is an almost constant companion of scleredema, lupus, rheumatoid arthritis.
parasitic infestations. Infection with parasites can provoke myositis. So, muscle inflammation is observed with toxoplasmosis, cysticercosis, trichinosis, less often with echinococcosis. When the parasite enters the muscle tissue, an inflammatory process of a toxic-allergic nature starts.
The negative impact of toxic substances. Most often, people who abuse alcohol, take medications, and have suffered insect bites suffer from myositis. The mechanism of development of inflammation is the direct effect of poison, alcohols, drug components on the muscles. Substances that increase the risk of developing myositis are: colchicine, statins, alpha-interferon, corticosteroids, isoniazid, antimalarial drugs (plaquenil, delagil, quinacrine, etc.), cocaine, alcohol.
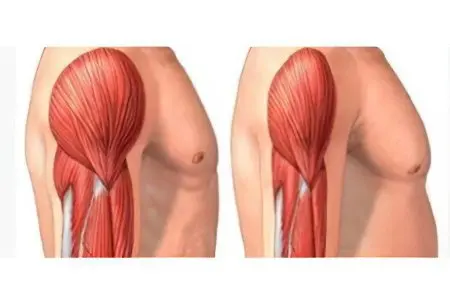
Postponed injuries. In the place where the rupture of muscle fibers occurs, inflammatory edema subsequently always increases, weakness and pain join. As the healing progresses, the swelling subsides, and normal muscle tissue is replaced by scar tissue, causing the muscle to become shorter. As a rule, myositis after minor injuries, hypothermia, muscle cramps or just intense physical exertion proceed quite easily. Rarely, a condition such as rhabdomyosis develops, characterized by necrosis of muscle tissue. Rhabdomyosis can be caused by dermatomyositis and polymyositis.
professional costs. Myositis often develops among pianists, violinists, PC operators, and drivers. The reason is prolonged stress on certain muscle groups or an uncomfortable body position. As a result, muscle nutrition suffers, normal blood circulation is disturbed, and dystrophic processes manifest.
Myositis symptoms
The symptoms of myositis are diverse, but its main manifestation is considered to be a muscular symptom complex, expressed in muscle weakness. It can disturb a person constantly and be quite pronounced, or it can appear only after a person performs certain tests. The loss of muscle strength occurs gradually, this process takes from several weeks to several months. Large muscles are involved in the inflammatory process – hips, neck, shoulders, back. Muscle myositis is characterized by bilateral symmetrical inflammation. At the same time, a person is not able to lift weights, climb stairs, and sometimes even just raise his hand and get dressed on his own.
The hardest people endure is myositis of the shoulder and pelvic muscles. Such patients often suffer from gait disturbance, have difficulty getting up from the floor or from a chair, and may fall during movement.
Other symptoms of myositis may include:
The appearance of a rash.
Increase in general fatigue.
Thickening and thickening of the skin.
Aching pain that increases with movement and probing of the muscles.
Sometimes there is hyperemia of the skin and swelling in the affected area.
Perhaps an increase in body temperature, feverish conditions, headaches.
Pain in the joints appears during periods of exacerbation of myositis, but the skin over the joints does not become swollen or hot, as in arthritis or arthrosis.
Myositis may have an acute onset or may have a chronic course. The acute phase can turn into a chronic one. Often this is observed with insufficient treatment or in the absence of therapy at all. Acute myositis occurs after trauma, after severe muscle strain or after hypothermia.
A chronic disease is characterized by an undulating course with increased pain during weather changes, with muscle strain. Sometimes there is a slight limitation of mobility in adjacent joints.
Types of myositis
It is customary to distinguish the following types of myositis, characterized by various manifestations:
Myositis of the neck. Pain in neck myositis occurs several hours after exposure to a provoking factor. Painful sensations tend to intensify during a person’s attempt to turn his neck or tilt his head. Possible irradiation of pain in the head, shoulders, back and shoulder blades. The pains do not become weaker after a period of rest, do not leave a person when he is motionless. Reddening of the skin over areas of inflammation is possible. When exposed to cold, the patient’s condition worsens.
Myositis of the back. Pain tends to increase in the morning, after a person spends a long time without movement. At night, there is an increase in tissue swelling, reflex muscle spasms. As a rule, back pain appears a few days after exposure to a provoking factor and persists for a long time after its elimination. Any physical activity – tilts, turns and other movements, accompanied by muscle stretching, leads to increased pain.
Myositis of the legs and arms. This type of myositis is rare without the involvement of other skeletal muscles located in other parts of the body. Most often, the muscles of the lower and upper extremities become inflamed with polymyositis. It becomes difficult for the patient to move, raise his hands up.
Myositis of the thoracic region. Myositis of the thoracic region is quite common. The pain syndrome constantly haunts a person, since the patient is not able to limit the movements of the chest resulting from breathing.
If myositis of the thoracic region is severe, then the muscles of the larynx and pharynx are involved in the pathological process. This contributes to difficulty swallowing, coughing and shortness of breath. It becomes difficult for a person to take a deep breath. In extremely severe cases, it is possible to involve the respiratory muscles in the pathological process, followed by fibrosis of the lung tissue.
Myositis of the eye muscles. Myositis can affect the muscles of one or both eyes. The pain gets worse when you try to look sideways or up. The eyelids swell, it is not possible to open them completely. Probably the development of unexpressed exophthalmos. If the disease becomes chronic, there is a possibility of developing restrictive myopathy.
Polymyositis. Polymyositis is most often diagnosed in people who have a predisposition to systemic diseases. Scientists suggest that the transferred viral infections, as well as oncological diseases, can become a trigger mechanism for the development of inflammation. By producing specific antibodies against them, the immune system sends them to fight with their own tissues. A process called rhabdomyolysis is started, characterized by damage to muscle fibers. Rhabdomyolysis is accompanied by an inflammatory process that tends to spread to adjacent tissues. In this regard, polymyositis is so often accompanied by joint pain, dermatitis and arthritis.
Polymyositis with symptoms of dermatitis is called dermatomyositis. This process begins acutely, can affect both adults and children. In addition to the main symptoms of myositis, dermatomyositis is characterized by the appearance of rashes. The rash has a purple or lilac color, slightly rises above the skin. Rashes are located on the neck, torso and face. Internal organs with polymyositis are rarely affected, but it is possible that the lungs, heart, gastrointestinal tract, and endocrine system are involved in the pathological process.
With juvenile dermatomyositis, the child begins to complain of pain in the lower extremities that appear when walking. Particularly painful areas of the leg in the region of the shins. Often, the development of an acute form of juvenile dermatomyositis is preceded by a sore throat or a cold.
Dermatomyositis is diagnosed twice as often in women than in men and is a systemic connective tissue disease.
Neuromyositis. Neuromyositis is a subspecies of polymyositis, but at the same time, both muscles and nerves, which are located in the area of inflammation, are involved in the process. As the disease progresses, inflammation spreads to the distal nerve fibers.
The patient experiences the following symptoms:
Deterioration of sensitivity (paresthesia), or an increase in sensitivity (hyperesthesia).
Severe pain.
Feeling of muscle tension.
Decreased muscle strength, decreased muscle tone.
Joint pain.
Pain in neuromyositis tends to increase as the disease progresses. Over time, the pain ceases to recede, even when a person is at rest.
Polyfibromyositis. Polyfibromyositis is another subspecies of polymyositis, which manifests itself in the fact that muscle tissue is replaced by connective tissue. This is due to the fact that muscles that have been in an inflamed state for a long period of time begin to break down. In their place, scar tissue forms in the form of nodules that can be felt. If scars form in the area of the tendons, then the appearance of contractures and deterioration of muscle mobility are not excluded.
Symptoms of polyfibromyositis may include:
Compaction of muscles located in the area of inflammation.
The appearance of nodules.
Abnormal muscle contractions.
Reducing the range of motion.
More than 20% of patients complain of difficulty in swallowing food.
Muscle soreness, especially on deep palpation.
Polyfibromyositis is characterized by the fact that the nodules can appear and disappear on their own, without any treatment. If the process of formation of contractures has started, then muscle deformation occurs, accompanied by severe pain. Most often, older people suffer from this type of disease.
Myositis ossificans. Myositis ossificans is one of the rarest types of polymyositis that occurs as a result of an injury: a dislocation, bruise, sprain or rupture of a muscle, or after a bone fracture. Thus, myositis ossificans of the thigh is often observed in riders, and chest myositis in fencers. In addition, this type of disease can be congenital.

Myositis ossificans is the result of untreated polyfibromyositis. The cicatricial tissue areas that appeared due to it are transformed into a mass with heterogeneous contents, which is impregnated with minerals and other substances (salts of phosphate acid, calcium, potassium). When there are too many minerals, the process of ossification starts. If the muscles with ossified areas are located in close proximity to the skeletal bones, then the latter are deformed.
The following symptoms may indicate myositis ossificans:
Deformity of the hands and feet.
The presence of muscle areas with uncharacteristic seals.
Mobility disorder.
The appearance of severe pain, prone to increase during movement.
During palpation, hard, hard areas of muscle are found that are similar in density to bones. As the disease progresses, a complete loss of motor activity of the limb is possible.
If myositis ossificans resulting from an injury has a favorable course, then the hereditary variety of the disease begins spontaneously and is characterized by an unpredictable prognosis. The death of the patient often occurs from ossification of the pectoral and swallowing muscles.
Lumbar myositis. Lumbar myositis is widespread. Patients often confuse this disease with lumbago, but pain in myositis is less acute. It is aching in nature and does not stop even when a person is at rest. Increased pain occurs with pressure on the lumbar zone, as well as during movements: bending, turning the body, etc.
Lumbar myositis must be differentiated not only from osteochondrosis, from kidney disease, but also from a hernia of the lumbar. To do this, the doctor should pay special attention to the symptoms of the disease, conduct an X-ray examination, MRI or CT.
This type of myositis is most often diagnosed in the elderly and in office workers.
Myositis classification
The classification of myositis can vary. So, depending on the nature of the course of the disease, chronic, acute and subacute myositis are distinguished, and depending on the prevalence: limited and generalized.
In addition, scientists note such special forms of myositis as:
Infectious non-purulent with severe pain and general malaise. This form develops during viral infections.
Acute purulent with the formation of purulent foci in the muscles, with their swelling and severe pain. This form of myositis is often a complication of existing purulent processes, or acts as a symptom of septicopyemia.
The parasitic form of the disease is the result of a toxic-allergic reaction of the body.
Myositis ossificans may be congenital or acquired as a result of trauma.
Polymyositis is expressed in multiple lesions of muscle tissue.
Dermatomyositis, called Wagner’s disease, is a systemic disease.
What is the danger of myositis?
The danger of myositis lies not only in the fact that the disease disrupts the quality of life of the patient, limiting his freedom of movement, but also threatens to develop more severe consequences.
Complications of myositis are:
The spread of the disease to neighboring muscles with the involvement of vital organs in the pathological process.
Atrophy of muscle tissue. If the disease progresses and is not treated, then a complete loss of working capacity is possible with the appearance of a need for systematic care.
Ossification of muscle fibers, which can eventually lead even to the death of the patient.
Breathing and swallowing disorders, if the muscles of the larynx, esophagus, pharynx are involved in the process of inflammation.
Complications of cervical myositis can be extensive lesions of the ENT organs, followed by shortness of breath and stress on the cardiovascular system.
Purulent myositis often leads to abscesses, phlegmon, which is a threat to human life.
How to treat myositis?

Treatment will primarily depend on the severity of the symptoms of the disease. It can be reduced to taking antibacterial drugs, antiviral agents, immunosuppressants, etc.
The treatment regimen for myositis should be selected on an individual basis, taking into account all the clinical manifestations of the disease.
To eliminate the inflammatory phenomena that provoked myositis, it is possible to use immunosuppressive drugs. If myositis is of a viral nature, then treatment should be aimed at maintaining the body’s immune forces and fighting the infection, since there is no etiological therapy. If the cause of inflammation of the muscles is a bacterial infection, then it is advisable to take antibiotics.
When myositis occurs against the background of taking medications, then their cancellation is necessary. Muscle fibers, as a rule, return to normal after 14-21 days.
Separately, it is worth noting physiotherapeutic methods for the treatment of patients with myositis. They are a prerequisite for the recovery of the patient, and without them the therapeutic course will not be complete. Physiotherapy allows you to increase muscle tone, prevent their atrophy and improve the patient’s well-being.
Physical activity must be present daily. It is worth visiting the pool, as swimming has a positive effect on all muscle groups.
You should adhere to the following recommendations of experts:
Before starting any physical work, the muscles need to be warmed up. This will normalize blood flow and speed up the work of the heart.
You can not overstrain, all exercises should be performed at the pace that is optimal for a person.
After exercise, rest should follow.
The pace should increase smoothly.
It should be concentrated on the inflamed muscle, in the event that the diseased area is too overextended, it is necessary to stop exercising and rest.
At a time when well-being is severely disturbed, the training program should be somewhat simplified.
It is better if the classes are held in pairs.
There is no specific training regimen for myositis, they are recommended to each patient individually. This takes into account the severity of the disease, the affected area, the age of the patient.
Special attention is paid to water aerobics. Regular exercise allows you to quickly restore activity, increase muscle tone.
As for drugs, research is constantly ongoing in this area and in the near future new drugs will appear that will more effectively get rid of myositis.
As a rule, people with various types of polymyositis most often either completely or partially restore lost muscle activity and tone. Therapy of fibromyositis does not allow you to fully get rid of the disease, but its progression slows down significantly if all the doctor’s recommendations are followed. Such patients manage to do without wheelchairs and other devices for movement for a long time. Against the background of concomitant diseases, such as oncology and pneumonia, the prognosis is much worse.
Infectious myositis will be more successfully cured, the sooner therapy is started. Therefore, at the first symptoms of muscle inflammation, you should immediately consult a doctor.










