Contents
What is gastroduodenitis?
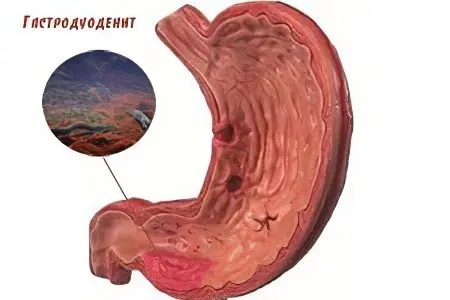
Gastroduodenitis – inflammation of the mucous membrane of the stomach and duodenum. In fact, this is a more severe form of gastritis, in which the pathological process passes to the underlying organ – the duodenum, which is fraught with aggravation of digestive disorders.
Most often, gastroduodenitis is diagnosed in the age group of 30-35 years, and its symptoms are more like manifestations of peptic ulcer than gastritis.
Gastroduodenitis is divided into acute (short-term, recent severe pain) and chronic (systematic aching pain in the upper abdomen). In chronic gastroduodenitis, large-scale violations of secretory and motor-evacuation functions occur, followed by a complete restructuring of the gastric mucosa.
How is gastroduodenitis different from gastritis?
There are no significant differences between these pathologies: both gastritis and gastroduodenitis are inflammatory diseases of the gastrointestinal tract. The only difference is that in gastroduodenitis, the area of lesion of the mucous membrane is wider than in gastritis, it also captures the duodenum. A possible cause of the development of gastroduodenitis, gastritis and stomach ulcers is infection with the bacterium Helicobacter pylori. Diagnosis and treatment of these diseases is practically the same.
Causes of gastroduodenitis

Allocate endogenous and exogenous causes of gastroduodenitis. With increased acid formation and low production of mucus, a violation of the hormonal regulation of secretion, endogenous gastroduodenitis develops. Also, diseases of the liver and biliary tract, malfunctions of the endocrine system can cause the development of gastroduodenitis.
Exogenous factors of development include physical ones – for example, the use of spicy, cold or hot food, exposure to chemicals (pesticides). Of no small importance is the penetration into the digestive tract of the bacterium Helicobacter pylori.
The main causes of gastroduodenitis include:
Poor or very fatty and spicy food;
Non-compliance with the diet, eating dry food;
Various stresses, psychological pressure;
Helicobacter pylori infection;
Infections that developed in the oral cavity and pharynx;
Recently, it has been noticed that the causes of superficial gastroduodenitis may be a genetic predisposition to such diseases.
In addition, there are acute and chronic forms of gastroduodenitis, when periods of remission alternate with exacerbations.
The reasons for the development of an acute form of gastroduodenitis:
Toxic effects of chemicals and spoiled food, irritating the mucous membrane of the stomach and intestines;
The use of hot spices and seasonings;
High concentration of pesticide residues in food;
Complications of intestinal infections and chronic somatic diseases;
Increased production of hydrochloric acid in the stomach, combined with a decrease in the protective properties of the mucous membrane, occurring against the background of stress and eating disorders.
Approximately 65-70% of cases of gastroduodenitis is a chronic form of pathology.
Causes of chronic gastroduodenitis:
Heredity;
Helicobacter pylori infection;
Complication of acute gastroduodenitis;
Staying in constant stress mode;
Malnutrition with a deficiency of protein, vitamins and trace elements;
Violation of the diet;
Diseases of other organs of the gastrointestinal tract (intestines, pancreas, gallbladder);
Complications of somatic diseases (autoimmune and endocrine pathologies, blood diseases, liver and kidney failure);
Side effects of drugs (NSAIDs, glucocorticosteroids) against the background of long-term use;
Smoking and alcoholism.
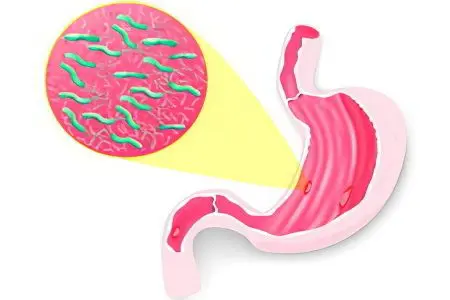
Each case of gastroduodenitis may have not one, but several reasons for its appearance. Several decades ago, after the discovery of Helicobacter pylori in 1983, approaches to determining the etiology of this disease have changed dramatically.
Flagella of active strains of a pathogenic bacterium are able to penetrate the epithelium of the gastric and intestinal mucosa damaged by it, and its enzymes break down the membrane proteins. The urease secreted by Helicobacter pylori disrupts microcirculation in the tissues of the gastrointestinal tract, hydrochloric acid ions damage the capillaries of the blood vessels of the stomach and intestines. All these aspects contribute to the development of inflammation.
Normally, the bacterium is found in the gastrointestinal tract of almost every person, getting there in childhood.
Helicobacter pylori manifests its destructive function due to a combination of the following factors:
Violation of the nervous and endocrine regulation of the functions of the gastrointestinal tract;
Increased acidity of gastric juice and impaired production of its protection in the form of mucus;
Imbalance of the AKUD system, which produces biologically active substances and hormones;
Violation of the regenerative functions of the mucous membrane of the stomach and intestines.
Symptoms of gastroduodenitis

Symptoms of gastroduodenitis in children and adults are different, but as a result, the disease always leads to a complex lesion of the gastrointestinal tract. This happens due to the fact that the duodenum produces hormones that have a significant impact on the secretory and evacuation activity of other organs of the digestive system. As a result of the progression of the disease, the stomach, pancreas, and biliary tract suffer. Most often, with chronic gastroduodenitis, a person feels aching cramping pains in the epigastric region. Frequent vomiting and regular heartburn begin to bother.
It is possible to make a diagnosis of “gastroduodenitis” if a person loses weight, he has a pronounced pallor of the skin, pain during palpation of the abdomen, a yellowish coating on the tongue and imprints of teeth on the inner side surface of the cheeks. In children, the symptoms are more pronounced. In addition, the child begins to suffer from vegetative and emotional disorders.
The clinical picture of the disease depends on the phase in which it is located – remission or exacerbation. In remission, the picture is very bright, the patient experiences intense pain for 10-14 days. With incomplete remission, pain does not bother, digestive disorders, heartburn, bloating, and heaviness are felt. During complete remission, the patient is not bothered by anything, signs of gastroduodenitis are detected during endoscopic examination.
The clinical picture of gastroduodenitis is similar to the symptoms of a duodenal ulcer: it is a pain, dyspeptic and asthenovegetative syndrome.
Pain syndrome

Adults suffering from chronic gastroduodenitis feel pain in the upper abdomen, in the projection of the stomach and duodenum 12, children under 10 years old in the solar plexus and in the navel.
Pain is usually associated with eating:
“Hungry pains” – felt in the morning, on an empty stomach, disappear after breakfast;
“Night pains” – occur during sleep, 4-5 hours after the last meal, disappear after eating;
“Late pain” – felt 1-3 hours after eating as a result of the receipt of a lump of food in the duodenum 12.
If the inflammation is localized in the intestines, “night” and “hungry” pains will be felt. With a predominant lesion of the stomach, the patient feels “late” pain. Another combination of pain syndromes practically does not occur.
Pain may be associated with psycho-emotional or physical overstrain, and not with food intake. The duration of the pain is different – from several minutes to 2-3 hours in a row. If it is enough to eat something to eliminate “hungry” pains, then “late” pains are eliminated much longer and more difficult.
Dyspeptic syndrome

With gastroduodenitis, digestive disorders associated with a disorder of the motor function of the stomach and intestines are frequent. As a result, food stays too long in the stomach and does not reach the small intestine in time.
Complex of symptoms of dyspeptic syndrome:
Feeling of heaviness and fullness of the stomach;
Heartburn;
Burping;
Fast saturation;
Bitterness in the mouth;
Bloating, flatulence;
Alternating constipation and diarrhea;
Nausea, rarely vomiting;
Slippage syndrome – defecation immediately after eating, is more often diagnosed in children.
Diarrhea is typical with inflammation of the stomach, constipation – with an inflammatory process in the duodenum 12. Bloating often occurs against the background of a combination of gastroduodenitis and pancreatitis.
In children suffering from gastroduodenitis with high acidity, increased sweating is found.
Asthenovegetative syndrome

It is most strongly manifested in severe pain and dyspeptic syndrome.
Characteristic features:
emotional lability;
fatigue;
Weakness;
lethargy;
Strong sweating in the limbs;
Rare pulse (below 50 beats per minute);
low blood pressure;
Red dermographism – the appearance of red spots on the skin with a strong pressure on it, remaining visible for half an hour.
Forms of gastroduodenitis
The grounds for isolating the forms of the disease are the intensity of the inflammatory processes occurring in the mucous membrane.
Types of gastroduodenitis:
Superficial – swelling and thickening of the mucosal folds appear during the acute period;
Hypertrophic – against the background of edematous and thickened mucosa, hyperemia, white plaque, punctate hemorrhages are diagnosed;
Mixed – the symptomatology is similar to the manifestations of hypertrophic gastritis, but has a more vivid clinical picture, in addition – the mucosa atrophies due to poor nutrition, its folds flatten;
Erosive – precedes the development of an ulcer, on the mucosa there are many erosions covered with mucus and a film of fibrinous plaque.
Classification of gastroduodenitis according to the degree of acidity:
With increased secretory function (diagnosed more often than others);
With normal secretory function;
With reduced secretory function (accompanies stomach cancer).
Up to 40% of cases of the disease may have an atypical manifestation, be asymptomatic. The clinical picture may not match the severity of symptoms with changes in the gastrointestinal tract.
Methods of diagnosis

A gastroenterologist can diagnose gastroduodenitis by conducting an examination or the necessary studies: esophagogastroduodenoscopy, if necessary, with a biopsy of the gastric mucosa.
It is also necessary to conduct a study of gastric secretion – pH-metry of the stomach and duodenum. Based on the results of these tests, it is possible to determine what form gastroduodenitis has – with increased or decreased acidity, and, accordingly, prescribe the correct treatment.
Modern methods for diagnosing gastroduodenitis:
Fibroesophagogastroduodenoscopy (FEGDS) – an accurate and informative method of endoscopic examination of the stomach and duodenum 12 using an endoscope, allows you to assess the severity and nature of damage, the form of gastroduodenitis.
Morphological study of mucosal tissuestaken during FEGDS – carried out using a microscope at the cellular level, allows you to diagnose the form and features of the disease.
X-ray examination with a contrast agent of the stomach and duodenum 12 – the method is less informative than FEGDS, it is rarely used.
Intragastric pH-metry – measuring the acidity of gastric juice using electrodes inserted into the stomach helps to determine the treatment regimen.
Bifrequency intragastric impedancemetry – measurement of the activity of the glands that produce hydrochloric acid, accurately determines the acidity of gastric juice.
Ultrasound of the stomach and intestines – an uninformative method that allows you to determine the indirect signs of gastroduodenitis.
The “gold standard” for diagnosing the disease is endoscopy of the stomach and duodenum, an additional informative study is the measurement of gastric acidity.
Treatment of gastroduodenitis
The main methods of treating the disease are diet therapy in combination with medication. Additional methods – psychotherapy, physiotherapy, restorative procedures.
dietary treatment:
Diet No. 1 – with exacerbations of chronic gastroduodenitis against the background of increased or normal acidity;
Diet number 2 – with exacerbations against the background of low acidity;
Diet No. 15 – with remissions against the background of normal health;
Diet number 3 – with constipation against the background of remission;
Diet number 4 – with diarrhea against the background of remission.
The treatment regimen for the disease depends on the etiology of gastroduodenitis. So, if Helicobacter pylori is detected, antibiotics are necessarily prescribed, in the absence of bacteria in the stomach, antibacterial agents are not used.
The main drugs in the treatment regimen for the disease are antacids and antisecretory drugs.
Gastroprotectors accelerate the regeneration of the mucous membrane of the stomach and duodenum 12. They contribute to the production of mucus that protects the walls of the stomach from the aggressive effects of hydrochloric acid, restore the structure of the mucous membrane. Gastroprotectors stop pain, eliminate heartburn. From spasms and severe pain in gastroduodenitis, drugs from the group of antispasmodics are used.
Therapy of the disease takes an average of 8-10 weeks, in a shorter period it will not be possible to achieve a stable remission. The course of treatment should not be interrupted even after the elimination of the main symptoms, it should be completed. Symptomatic remedies are used as needed – the presence of diarrhea, constipation, heaviness in the abdomen, with heartburn, pain. If there are no pronounced symptoms, only antacids and antisecretory drugs are used.
For the treatment of a mild form of the disease, one course is enough; in severe cases, several courses are used. Between them make a 2-5-month break, then repeat the treatment. The frequency of courses of therapy is determined by the attending physician.
What is recommended to eat with gastroduodenitis?
Soups cooked on vegetable, mushroom, fish broths, mashed;
Lean meat (chopped, baked) boiled chicken;
Steamed cutlets, stewed, fried, but without a rough crust;
Low-fat ham;
Boiled fish, chopped low-fat herring, pre-soaked;
Milk (if there is no diarrhea), butter, kefir, yogurt, cream, non-acidic sour cream, fresh non-acidic cottage cheese, mild cheese;
Soft-boiled eggs, scrambled eggs;
Porridges, boiled or mashed (buckwheat, semolina, rice);
Flour dishes: stale white, gray bread, lean crackers (exclude baking);
Vegetables, non-acidic fruits;
Vegetable and fruit juices;
Weak tea, coffee, cocoa on the water with milk.
If symptoms of gastroduodenitis appear, you should contact a gastroenterologist for diagnosis and treatment. Exact adherence to the recommendations of the doctor will help to quickly cope with the disease.









