Contents
What is osteomyelitis?
Osteomyelitis – this is an infectious inflammation of all the constituent parts of the bone tissue: bone, periosteum and bone marrow. However, not only the bone suffers, but also the bone marrow, the softest component, increases and swells. The hard shell begins to put pressure on the tissue, as a result of which the blood vessels are pinched, and there is a loss of blood flow in the damaged area. This, in turn, often causes destructive processes. And if the causative agent of the disease penetrates beyond the bone, for example, into the muscles, then an abscess may develop – filling the cavity with pus.
The symptom is osteomyelitis

The most dangerous osteomyelitis, the cause of which is an internal infection. The disease develops in just 2 days. During these days, the symptoms of the disease are hardly noticeable. Perhaps a general malaise, muscle pain, discomfort in the joints, a person does not even suspect that he is developing osteomyelitis. Then the body temperature rises to forty degrees. There is severe pain in the area of the affected bone. When moving, the pain intensifies, the movement becomes limited. The disease further develops rapidly. Very often this whole process is accompanied by a sharp deterioration, nausea and the urge to vomit.
The main danger of asymptomatic osteomyelitis is the lack of treatment and the possible transition of the disease from a local form to a generalized one, from an acute stage to a chronic one. Therefore, any unusual sensations, fever without other accompanying symptoms require diagnosis and investigation.
With osteomyelitis with a toxic form of the disease, pressure drops, pain in the heart is felt, convulsions and loss of consciousness are possible. The face becomes pale, the eyes sink, the skin turns yellow, the lips turn blue. When a traumatic form of osteomyelitis appears, it is very important to immediately consult a doctor, otherwise the person may die.
Traumatic osteomyelitis is characterized by acute symptoms. Both high temperature and severe pain in the area of injury are possible, after which all these symptoms are replaced by chronic ones. A person feels more or less normal, various purulent discharges are excreted through the fistulous passages that occur in the wound area and are the first cause of traumatic osteomyelitis. A severe form of osteomyelitis can result in blood poisoning.
According to clinical manifestations, osteomyelitis is divided into two types:
local;
generalized.
The following symptoms are characteristic of the local course of the disease:
An increase in body temperature up to 38,5 ° C.
The formation of swelling, elevations in the damaged area.
Aching, pain, which is bursting in nature.
The skin on the problem area heats up and turns red.
The appearance of abscesses.
Discharge of pus through the skin.
Pain and limited movement.
The generalized form is manifested by several other signs:
the temperature rises to 39–40 degrees;
the pain intensifies, becomes permanent;
general intoxication increases (general poor health);
chills, sticky sweat, hoarse shortness of breath appear;
neurological lesions (convulsions, delirium, loss of consciousness);
kidney disorders (painful and frequent urination);
pallor of the skin.
Causes of osteomyelitis

The main causative agents of acute osteomyelitis are staphylococci, but other bacteria, rickettsia and some fungi are also possible, which enter the bone tissue and provoke the onset of the disease.
The main “fault” lies with Staphylococcus aureus, but some Escherichia coli, hemolytic streptococcus and Pseudomonas aeruginosa can also cause the disease. The disease can be caused either by a single pathogen or by a group of pathogenic microorganisms.
In order for the inflammatory process to begin, some factors are necessary: predisposing and triggering mechanisms.
Factors that predispose to osteomyelitis include:
hidden infections;
allergic diseases;
weakening of the immune defense;
physical exhaustion;
a long period of fasting and a lack of nutrients in the body.
Mechanisms that “trigger” the disease:
various injuries;
burns and frostbite;
ARVI;
excessive physical exertion;
violations of the general psycho-emotional state (stress, prolonged nervous exhaustion).
There are three types of infection:
through the blood supply
direct contact with pathogens (for example, with a burn, injury);
transmission of infection from adjacent parts of the body.
The risk factors include:
tuberculosis;
ulcer;
trauma;
any damage caused by thermal burns;
circulatory disorders;
infectious diseases of the nasal sinuses, oral cavity, dental ailments;
Diabetes;
oncological diseases and their treatment (chemotherapy);
surgical interventions.
Hematogenous (“blood-borne”) osteomyelitis is common in infants and young children. From the focus of infection – for example, from a diseased tooth – microbes penetrate into the bone marrow canal of the long tubular bone of the arm or leg. Rarely, osteomyelitis is caused by a soft tissue infection that spreads to adjacent bone. One of the causes of osteomyelitis can be an open fracture, in which case the infection penetrates through the laceration into the bone.
Why osteomyelitis occurs, experts still do not know. There are three theories regarding the mechanisms of the development of the disease (vascular, neuro-reflex, allergic), but none of them has been confirmed enough to be considered true.
Acute osteomyelitis
Depending on how the pathogen penetrated into the tissues, acute osteomyelitis is divided into endogenous and exogenous forms. The endogenous (or hematogenous) type is characterized by infection through the circulatory system from other foci of the disease under the influence of trigger factors.
The exogenous species include:
contact;
post-traumatic;
gunshot;
postoperative.
Acute hematogenous osteomyelitis
The method of infection is the “classic” introduction of pathogenic bacteria into the blood vessels inside the bone, as a result of which the primary focus of the disease occurs. Children aged 3 to 15 years are most at risk, but it is also common in newborns, middle-aged and elderly people. Hematogenous osteomyelitis affects males more and most often in the period from spring to autumn. The hematogenous form has a special “love” for long bones: the femur, tibia, and shoulder.
According to the nature of the course of the disease, 4 forms of hematogenous osteomyelitis are distinguished:
Break, the most favorable and easy form. With such a course, the body activates all protective functions and recovery systems and eliminates the focus in 2–3 months.
Protracted, which lasts much longer than break, up to 6-8 months. But, although the recovery process is long, the disease recedes over time.
Lightning, the most severe and unpredictable form of hematogenous osteomyelitis. Most often it is provoked by a staphylococcal infection and is characterized by a one-time release of bacterial decay products (in this case, endogenous) into the blood. The strength of the influence of the ejection is such that in a matter of minutes, blood pressure drops to almost zero. And without the provision of urgent, momentary assistance, a fatal outcome occurs.
Chronic, with a long course of more than 8 months. It is characterized by relapses (splash of the disease) and remissions (attenuation of inflammation). It is often accompanied by the formation of sequesters – special dead tissue areas that prolong inflammation. Fistulas are formed, which open according to relapses and close during remissions. The chronic stage can lead to muscle atrophy and amyloidosis (violation of protein metabolism in the body).
There is another form – primary chronic, which is increasingly common in recent years.
Experts attribute the increase in the number of sick people with this form of osteomyelitis to the following factors:
with malnutrition;
with insufficient intake of important trace elements in the human body;
with the environmental situation worsened over the past decades;
with irrational and widespread use of antibacterial agents;
with limited mobility.
The primary chronic form is divided into the following types:
abscess Brody;
albuminous;
antibiotic;
sclerosing.
Primary chronic osteomyelitis is characterized by a rather sluggish course, which makes it difficult to make a correct diagnosis.
Acute odontogenic osteomyelitis
The odontogenic type is an infectious lesion of the jaw bones with the formation of a purulent-necrotic process. The vast majority of patients with this type of osteomyelitis are men over the age of 35. Damage to the lower jaw develops more often, up to 85%, upper – up to 15%, and damage to the maxillary tissues proceeds much more easily.
Among the reasons for the appearance can be identified:
general decrease in immunity;
errors during surgical dental intervention;
dental diseases (dental cysts, periodontitis);
diseases of the nasopharynx (frontal sinusitis, ethmoiditis, sinusitis);
metabolic disease;
a sharp increase in the number of conditionally pathogenic microorganisms;
direct infection due to trauma and thermal damage.
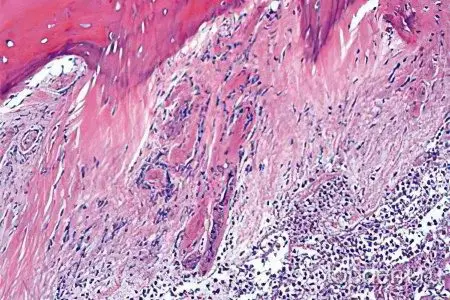
The development of the disease is accompanied by the formation of small hemorrhages due to the occurrence of thrombosis of the blood vessels of the bone tissue. Because of this, purulent foci of various sizes begin to appear, and the death of individual tissue sections is provoked. In addition, isolated foci of necrosis often occur, in which case they speak of nosological forms of odontogenic osteomyelitis.
The disease is manifested by acute pain with intense impact in the area of the temples, sinuses, forehead. The side of the jaw on which the focus of infection is located begins to hurt. The body temperature rises, there may be increased sweating, chills and a general disturbance of well-being.
Chronic osteomyelitis

In the case of advanced acute osteomyelitis, untimely response, a subacute period occurs, which turns into a chronic stage. It is characterized primarily by the duration of the disease, significantly exceeding 2–3 months to 8–12 months, sometimes several years. In the chronic form, the formation of sequesters and fistulas occurs. There is an alternating change of exacerbations and attenuation of the disease.
Chronic odontogenic osteomyelitis
Approximately one week after the acute onset of odontogenic osteomyelitis, a subacute stage develops, which, after 3-5 days, becomes chronic. Causes of the transition of the disease from the acute stage to the chronic stage:
general decrease in the body’s defenses;
hypothermia;
overwork;
acute respiratory diseases;
incorrect actions during the elimination of the acute odontogenic period.
Symptoms:
elevated subfebrile (around 37,5) temperature;
slight malaise and weakness;
the formation of fistulas and sequesters;
discharge of pus and sometimes small areas of dead tissue through fistulous openings;
lack of sleep.
On radiographic images and the results of computed tomography, alternations of healthy tissue sections with lesions of various shapes and sizes are clearly visible.
Hematogenous chronic osteomyelitis
When the acute stage passes into the subacute, and then into the chronic, the temperature drops to subfebrile indicators, sometimes it normalizes. Excessive pain disappears. The affected area is compacted, limited in movement and swollen. In the area where there was a surgical incision, a fistula is formed through which pus is released. Sometimes spontaneous tissue rupture occurs, followed by the formation of multiple fistulas. Often they exist for months or even years. Single large sequesters or small group formations of dead tissues are formed.
If the pus does not find a way out and accumulates under soft tissues, swelling occurs in this area, the skin becomes hot to the touch and turns red, pain and fever appear. When the fistula opens and the pus comes out, the symptoms disappear.
For diagnosis, radiography is used, which can detect changes as early as 12–14 days after the end of the acute stage. At this stage of the disease, the method of fistulography, which is a computed tomography using a contrast agent, is very informative. A clear image allows you to determine the size of sequesters, their localization, the overall severity of the disease.
How serious is osteomyelitis?
After the doctor makes a diagnosis, a qualified consultation is carried out, patients mistakenly assume that osteomyelitis is a simple inflammation that has affected a small area of uXNUMXbuXNUMXbthe bone and has absolutely no effect on other processes occurring in the body. Therefore, a person does not understand the seriousness of the disease that has arisen in them, they are not serious about its treatment, which leads to serious complications, and sometimes even death. For this reason, it is necessary to explain to the patient how dangerous this disease is and what consequences it can lead to.
Particular attention should be paid to the fact that during osteomyelitis, the work of the liver and kidneys significantly deteriorates, there is a general depletion of the body, and the functioning of the immune system worsens. It happens that a person dies not from osteomyelitis itself, but from diseases that are caused by it, especially when those organs are affected that were not completely healthy before this disease.
Diagnosis of osteomyelitis
On examination, a careful palpation (palpation with fingers) of the painful area is carried out, while the condition of the skin is noted (hot, there is redness and swelling, wave-like movements of the tissues are formed) and the general appearance of the damaged area (stretched skin, “glossy” shine, puffiness). With the help of careful percussion (tapping), the focus of infection is determined by increasing pain in a specific place of swelling.
In addition to the assessment of clinical manifestations and manual examination, laboratory research methods are used:
A general blood test with a leukocyte formula in expanded form shows a shift to the left. This means that the inflammation in the body is caused by a bacterial nature. Neutrophils are responsible for its suppression, of which there are 4 forms (segmented, stab, young neutrophils and myelocytes). When the formula is shifted to the left, an increase in segmented neutrophils and the appearance of stab individuals are noted. The more acute and severe the infection, the more youthful forms of neutrophils appear in the analysis. In addition, parameters such as ESR – erythrocyte sedimentation rate, hemoglobin and platelet levels reveal the nature of the course of the disease.
A general urine test shows the presence of inflammation and kidney failure (with generalized forms of the disease) by the appearance of protein, an increase in some indicators.
A biochemical blood test shows an inflammatory process and notes renal and liver failure. At the same time, the parameters of bilirubin and protein change, the glucose index decreases, and the amount of some elements increases.
Along with laboratory methods, instrumental examination methods are used:
Ultrasound examination used to assess the size and shape of a muscle lesion.
infrared scanning can show the presence of acute latent forms of osteomyelitis by identifying areas with elevated temperature.
X-ray is the most common diagnosis of osteomyelitis. With the help of images, it is possible to determine the localization of necrotic processes, the volume and severity of the infectious focus. With the help of x-rays, the disease can be detected in the early stages. As the inflammation grows, the nature of the image in the pictures changes, so the time of the course of the disease can be indicated with high accuracy.
Computed tomography – the most informative way to diagnose osteomyelitis in any of its manifestations. With the help of volumetric images, it is possible to obtain not only data on the localization and intensity of the infection, but also to create a reconstruction of the surrounding muscle tissues and predict the course of the disease.
For an accurate diagnosis, which is of decisive importance in the treatment of osteomyelitis, a combination of laboratory and instrumental research methods is necessary.
How is the treatment?
Measures for the treatment of osteomyelitis should be comprehensive and carried out in a timely manner. Constant monitoring of the disease in dynamics is necessary, since the course is often accompanied by unpredictable complications and variations in lesions. For a thorough fight against any form of osteomyelitis, simultaneous drug therapy, surgical interventions and a complex of physiotherapeutic procedures are recommended.
Principles of medical (conservative) treatment
The main point: the treatment of osteomyelitis only with medications without the intervention of surgical practice does not lead to the proper result. On the contrary, an insufficient concentration of antibacterial drugs provokes mutations of pathogens, as a result of which they become resistant to drug therapy.
With the help of an intraosseous infusion of a mixture of saline and antibacterial agents, the focus of infection is washed and a barrier is created around it, which prevents the spread of the pathogen outside the affected area. Moreover, washing helps to reduce pressure in the bone tissue, remove pus and relieve pain.
An antibacterial drug is selected one to which the type of pathogenic bacterium is sensitive. The medicine is injected into the bone cavity and applied in a course of 1-2 months. In some cases, the period of use of antibiotics is extended: up to 3-4 months. In general, the period of antibiotic therapy is determined by the severity and nature of the disease.
Important points:
For the period of treatment, it is recommended to carry out immobilization (limitation of mobility) of the damaged area using special devices. In general, reduce physical activity as much as possible.
In the case of a long course of drug therapy with antibiotics, agents are used to increase the overall resistance of the body. For this, infusion (intravenous) infusions of special solutions are carried out, blood preparations are used.
In cases of severe damage, ultraviolet exposure to the blood is connected.
When sepsis occurs, a number of measures are taken to cleanse the blood and lymphatic system of toxins.
In the process of treatment, careful monitoring of the electrolyte balance of the body is necessary.
A complex of therapeutic and physical exercises can be used only after the withdrawal of the patient from the acute period of the disease and the removal of the pain syndrome. With the help of physical therapy, the functions of damaged areas are restored, the activity of muscle tissue is stimulated, the affected area receives nutrients and vitamins.
Surgery

Surgical intervention is not possible with concomitant diseases in the decompensated stage: complications more serious than osteomyelitis may occur.
Indications for surgery for osteomyelitis:
atypical form;
purulent processes;
diffuse purulent inflammation (phlegmon) of the periosteum;
formed sequesters;
fistulas;
repeated recurrence of the disease.
The basic rule is to remove the purulent focus, regardless of its size. Preoperative preparation includes detoxification, administration of immune system supportive drugs, metabolic checks and, if necessary, the use of corrective drugs.
Surgery is performed under general anesthesia. Each operation includes specific stages of implementation, depending on the final goal and the desired result.
But in general, the course of surgical intervention looks like this:
First, the visible surgical field is processed with antiseptics and the instruments are checked.
The effect of anesthesia is assessed and, if the condition is satisfactory, the first incision is made.
With the help of subsequent incisions, the surgeon gets to the focus of infection, which in most cases has an intraosseous location.
Using special tools, a bone area is opened directly above the focus, commensurate with inflammation. If there are signs of purulent inflammation of the diffuse form, then purulent formations are first eliminated.
The next step is drilling small holes, resembling an elongated rectangle in location. Then, using an electric surgical jigsaw, the holes are connected by an incision, and as a result, a bone plate is obtained, which is removed. The bottom of the medullary canal opens, where the focus of osteomyelitis is concentrated.
The canal is washed with antiseptic solutions, a drainage tube with side armholes and a free edge is inserted into it, which is fixed outside the incision.
The final stage is suturing the wound in layers.
After the operation, using the installed drainage, the cavity is washed with antibacterial solutions and the contents are evaluated: if the discharge indicates the cleanliness of the intraosseous cavity, then the wound is reopened and the drainage is replaced with a section of striated tissue with an attached vessel for nutrition (surgical plasty). This is necessary to prevent recurrent osteomyelitis. And the drainage is installed already in the soft tissues. In the course of healing, it is removed.
Treatment of gunshot and chronic post-traumatic osteomyelitis
At the forefront in the treatment of osteomyelitis of gunshot origin is surgical radical intervention, during which foreign objects, bone fragments and dying tissues are eliminated. After that, the area around the wound is subjected to “chipping” with antibacterial drugs, and drainage is performed if necessary. At the end of surgery, the patient receives antimicrobial therapy, a complex of vitamin infusions, and measures to remove toxins from the body.
Chronic post-traumatic form of osteomyelitis is most often complicated by defects (fractures, bone shortening, false joints). Basically, to eliminate fistulas and join bone fragments, the osteosynthesis method is used, which consists in a clear fixation of broken sections in the correct anatomical position for subsequent fusion. In the case of the formation of phlegmon, the focus is opened, pus and necrosis are removed, and the cavity is drained.
Therapeutic exercise for osteomyelitis

After surgery, a course of exercise therapy for the damaged area can be carried out no earlier than 20 days after the operation. However, other parts of the body not involved in the operation need movement. Therefore, twice daily for 10-15 minutes, “exercises” are carried out to prevent the formation of bedsores and stimulate blood flow in the tissues.
Over time, the duration of the exercises is gradually increased, giving an increasing load and smoothly moving to the affected area. At the final stage of physical therapy, the emphasis is on returning the damaged area to the correct motor movements.
At the stage of recovery, physiotherapeutic procedures are also successfully used: electrophoresis, exposure to ultraviolet rays and ultra-high frequency therapy.
Nutrition Issues
A properly selected diet for osteomyelitis plays its own, often important, role in the complex treatment of the disease. It is recommended to divide the daily meals into smaller and more frequent meals for better absorption (5-6 times a day). The diet must include dairy products, meat products, eggs, fresh vegetables and fruits. Liquids require at least 2 and a half liters per day. Foods high in iron, calcium and protein are welcome. If the patient has concomitant diseases that require a special diet, all questions and appointments are discussed with the attending physicians.
Prognosis of the disease
In the process of making a diagnosis of acute or chronic osteomyelitis, a prognosis of the disease is made, which depends primarily on the form of the course of the disease and the patient’s condition before hospitalization. The age and state of immunity also play a role, and, of course, the stage of the disease and the timeliness of its detection. The sooner complex treatment begins, the greater the chances of a full recovery. An unfavorable prognosis is most likely in patients with chronic osteomyelitis in a neglected state and in combination with bone thinning.









