Contents
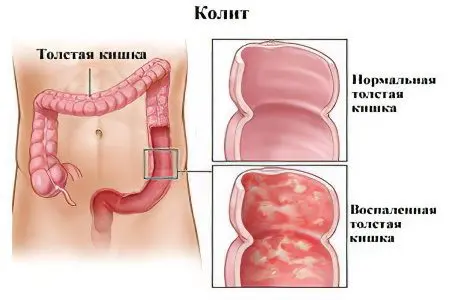
What is intestinal colitis?
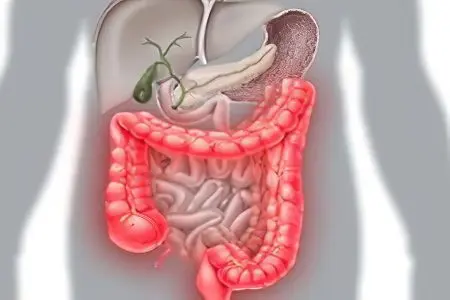
Colitis is an acute or chronic inflammatory process that occurs in the large intestine, which occurs due to toxic, ischemic or infectious damage to the organ.
In the view of the average layman without special medical knowledge, colitis is associated with intestinal colic. However, these two states are far from the same. Intestinal colic is an uncomfortable paroxysmal pain sensation in the lower abdomen. Colic is just a symptom that characterizes a huge number of diseases and pathologies, from banal flatulence to oncological processes.
Colitis, in turn, is an independent disease that differs in its own etiology, symptoms and features of the course.
To better understand what this pathology is, it is necessary to turn to the basics of the anatomy of the gastrointestinal tract.
The intestine is divided into two sections: the large intestine and the small intestine. Each has its own digestive functions. The thin section begins immediately after the stomach and the main digestive processes take place in it (including the final processing of food, the release of nutrients and their transportation to the bloodstream through the walls of the organ).
The small intestine is separated from the large intestine by a mucous membrane. Thanks to her, waste products and microorganisms from the large intestine do not enter the previous section. In the large intestine, the final processing of food and absorption of fluid takes place. Not the last role in this process is played by special bacteria (in the large intestine, their volume reaches about 1,5 kg or even more).
In the colon, in addition to the “beneficial” bacteria (which contribute to the processing of food debris), pathogenic organisms also live. These microorganisms in the course of life produce a huge amount of active substances with a high toxic potential. If, as a result of the consumption of low-quality food or for other reasons, the concentration of pathogenic microflora in the body grows, the colon mucosa becomes inflamed. This is how the immune reaction manifests in order to prevent the penetration of toxins into the bloodstream. colitis develops.
In some cases, pathogenic microflora can penetrate the small intestine, in which case an even more severe form of pathology develops – enterocolitis. It should be noted that if a conditionally useful microflora enters the small intestine, enterocolitis will not develop and everything will be limited to discomfort and bloating.
The etiology of colitis is not limited to infection. Some medications have the same effect (side effect), and colitis can also accompany some other pathological processes.
Colitis symptoms
The first signs of acute and chronic colitis differ significantly in intensity and degree of increase in symptoms.
Symptoms of acute colitis
Colitis in the acute phase is characterized by a rapid increase in manifestations and their high intensity. However, this is not an axiom, and much depends on the individual characteristics of the patient’s body (in particular, the characteristics of the immune system). In some patients, the symptoms are pronounced, the disease is severe. In others, slight discomfort is noted, and the pathology is characterized by a sluggish course.
Important factors in addition to the characteristics of the immune system are: the age of the patient, the degree of toxic, infectious or ischemic damage to the intestine, the presence of other concomitant pathologies.
Among the symptoms, the following are most characteristic:
Discomfort and pain. Often accompanied by a disease, aggravated after therapeutic procedures (enemas), eating, mechanical impact (for example, shaking in transport), walking or running.
Disorder and instability of the stool. This manifestation cannot be called the main or characteristic only for intestinal colitis. Diarrhea and constipation, as well as their alternation characterizes most gastrointestinal disorders, from cholecystitis to botulinum toxin poisoning. The main difference between the stool in colitis is the presence of colorless or greenish mucous streaks or blood impurities in it.
False urge to defecate (the so-called tenesmus). Characteristic not only for colitis, but also for a number of other diseases, such as, for example, proctosigmoiditis (inflammation of the sigmoid and small intestine) or proctitis. Discharge scanty, mucous. With the development of colitis in the colon, urges are relatively rare, patients are disturbed no more than 2-3 times a day. However, if the process is localized in the rectum or sigmoid colon, the urges are more painful, often occur at night and end with a small amount of excreted feces (like “sheep feces”) with abundant impurities of blood, mucus, and pus.
Heaviness in the abdomen.
Bloating.
Flatulence.
Symptoms of chronic colitis

If the treatment was started late, or carried out incorrectly, the disease may subside, turning into a chronic form.
Exacerbations can occur up to several times a year. Symptoms are similar to acute colitis. Even at the stage of remission, in 35-40% of cases, sluggish manifestations are observed.
Flatulence (increased gas formation).
Chair problems. In 80% of cases, we are talking about severe spastic constipation, which is associated with a lack of “useful” microflora and a violation of intestinal motility.
Rumbling in the abdomen, which occurs a few hours after eating.
Mild pain in the abdomen after exercise or stress.
– Skin rash caused by toxic damage to the body due to impaired excretion of feces.
Weakness, headaches, nausea.
Symptoms worsen during periods of exacerbation.
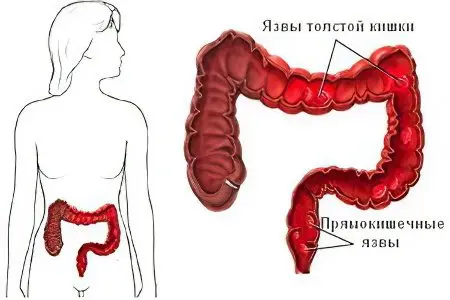
Symptoms of ulcerative colitis
Ulcerative colitis is a special case of intestinal colitis. Its main difference is the presence of ulcerative defects on the walls of the mucous membranes (up to perforation), which causes a much more severe pathology. Ulcerative colitis is characterized by a special symptomatology.
Frequent false urge to defecate. At the beginning of the process – meager diarrhea (up to 15-20 times a day), the inability to hold a chair. The symptom is observed in more than half of the patients (55-60%).
Foreign matter in the stool. Blood, greenish mucus, bands of pus. The discharge of blood varies from insignificant (found only on toilet paper) to abundant, visible to the naked eye in the stool.
sudden constipationindicating inflammation of the small intestine. It occurs in about a quarter of patients.
Manifestations of intoxication of the body. Manifestations are similar to SARS. In severe lesions, there is an increased heartbeat (tachycardia), general weakness, fever, nausea, vomiting, and decreased appetite. Diarrhea can also lead to dehydration.
In some cases, symptoms unrelated to lesions of the gastrointestinal tract may develop.. Visual disturbances, skin rash, itching of mucous membranes, blood clots, joint pain. In addition, the liver and gallbladder may suffer.
Pain in intestinal colitis
Pain in colitis of the colon is aching or dull in nature. Sometimes patients complain of bursting pains. Unpleasant sensations can be persistent and painful, but most often the pain is manifested by periods (cramping).
The localization of pain varies from case to case. Often it is impossible to determine the localization, the pain spreads throughout the abdomen or wanders. In the initial period, discomfort occurs in the lower left side of the abdomen.
The pain radiates to the back, sacrum, left side of the chest. For this reason, often the patient cannot independently determine the source of pain, taking colitis for problems with the spine or heart.
After taking drugs (antispasmodic, anticholinergic), discharge of intestinal gases, defecation, warming the affected area, the pain subsides, but after a certain period of time they return again. In some patients, passing gases, on the contrary, leads to increased pain.
Causes of intestinal colitis
The causes of intestinal colitis are currently unknown. Numerous scientific studies are being carried out, but scientists have not yet come to a consensus. Despite this, a number of provoking factors can be identified. They act as triggers that initiate the onset of the pathological process.
Infectious lesions of the body. It is quite trivial when a person consumes low-quality expired food. Food poisoning is caused by pathogenic microflora that actively multiplies in the intestines. In addition, under other conditions, a person can become a carrier of an intestinal infection, Vibrio cholerae, dysenteric amoeba, salmonella, and other infectious agents. Bacteria of tuberculosis, shigellosis can become such agents.
Malnutrition (alimentary causes of colitis). At the household level, colitis caused by a violation of the mode of consumption of food is called “indigestion.” Alimentary colitis is caused by excessive consumption of fast food, irregular meals, alcohol abuse, lack of fiber intake, insufficient intake of “healthy” food (vegetables, fruits, natural meat products), etc.
Genetic factors. Some genetic mutations can cause congenital disorders of the intestines.
The presence of comorbidities. Cholecystitis, hepatitis, pancreatitis, various forms of gastritis contribute to disruption of the intestines and the development of colitis. The same effect is produced by a decrease in immunity and a weakening of the body after a viral illness.
Taking medication. Many drugs adversely affect the intestinal microflora and reduce intestinal motility. Antibiotics, anti-inflammatory drugs, aminoglycoside drugs, laxatives, contraceptive drugs, etc.
Toxic poisoning. They can be both exogenous in nature (poisoning with mercury salts, phosphorus, arsenic) and endogenous (for example, poisoning with urate salts in gouty lesions).
Allergic reaction. Food and other forms of allergies contribute to disruption of the intestines.
Mechanical impact. Abuse of cleansing enemas or suppositories leads to disruption of the intestines due to constant irritation of the intestinal mucosa.
In all cases, pathogens secrete toxins that irritate the intestinal wall and cause specific symptoms. Despite the origin of the disease in this case, colitis caused by infection is considered non-contagious.
Forms of colitis of the intestine
Acute colitis of the intestine
The acute form of intestinal colitis is caused by one of the above reasons and proceeds in most cases rapidly with a gradual increase in characteristic symptoms.
Most often, acute colitis is provoked by food poisoning, an allergic reaction (as a result of which mast cells-basophils are destroyed and histamine is released in large quantities, violating the integrity of the cells of the intestinal mucosa, causing the intestines to become irritated), or excessive intake of certain medications.
The disease begins with the development of hyperthermia (the temperature rises to 37.2-38.1 degrees). The patient experiences weakness, following the temperature there are cramping pains and cramps in the abdomen. The large intestine along its entire length is painful and responds with dull pain when pressed.
The urge to defecate is frequent, accompanied by scant secretions of mucus or a small amount of liquid feces.
Pain attacks are accompanied by sweating, dizziness, pallor of the skin. There is a picture of intoxication of the body.
In addition to specific symptoms, there are also general phenomena on the part of the body.
A sharp drop in body weight by 2-6 kg.
Periodic increase in body temperature.
Drowsiness and fatigue.
nausea, vomiting.
These phenomena can persist for quite a long time after suffering acute colitis (up to 10-25 days).
If adequate treatment of the pathology has not been carried out from the very first days, colitis can become chronic with periodic relapses. With the transition of the disease to a different form, the symptoms also weaken and disappear by themselves.
Chronic colitis of the intestine
Gastroenterologists agree that the main cause of intestinal colitis is a violation of the diet. Therefore, among people aged 25 to 40 years, colitis is much more common than you might think.
In some cases, colitis caused by:
Complications of transferred infectious diseases of the intestine (salmonellosis, cholera, intestinal form of influenza, etc.);
Long-term exposure to the body of salts of heavy metals and toxic non-metals (typical for people working in hazardous industrial enterprises);
Dysbacteriosis, as a result of which the concentration of beneficial microflora and intestinal motility are disturbed;
Enzymatic deficiency as a result of diseases of the gallbladder, pancreas and stomach.
However, malnutrition remains the primary cause. Lack of fiber in the diet leads to a decrease in mucus secretion and disruption of the normal evacuation of feces from the colon. Stagnation of feces in the intestine leads to irritation and inflammation of the mucosa.
An unhealthy diet plays a significant role in the development of colitis (therefore, women are additionally a special risk group).
The chronic form is not necessarily preceded by a pronounced acute phase. A situation is possible in which there will be one single symptom of an acute form, and then very sluggish. In other cases, there may be no symptoms at all, then the pathology proceeds in the reverse order.
A bright and severe course of chronic colitis is possible only at an advanced stage.
The first symptoms to look out for immediately are:
dry mouth;
stool disorders;
Constant thirst;
Lack of appetite.
If the necessary treatment is not carried out, the disease will form completely, and the manifestations will subside.
Chronic intestinal colitis does not appear suddenly and out of nowhere. For the disease to manifest itself “in all its glory”, a trigger is needed, a trigger mechanism. Such a trigger can be food poisoning, infection, trauma, an allergy attack, etc.
Only in 10-12% of the total number of patients, after the development of a trigger, colitis does not manifest itself, but subsides and gradually heals spontaneously, in other cases this unpleasant pathology becomes a lifelong companion of a person.
During periods of exacerbation, there is a picture of an acute form of pathology, however, as was said, specific symptoms (albeit in a weakened form) accompany the patient even during remission.
Types of intestinal colitis
ulcerative colitis of the intestine

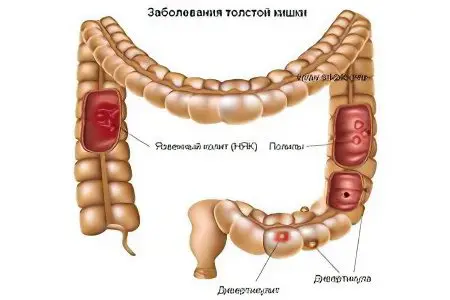
Ulcerative colitis of the intestine is an inflammation of the mucous membrane of the colon, accompanied by ulceration of its surface, edema and degenerative changes in the epithelium of the membrane.
The high-risk group includes young people aged 20 to 40 years, as well as older people (after 50-55).
The pathological process is characterized by ulceration of the walls of the large intestine throughout the organ.
The etiology of this type of colitis is not completely known, at the moment a number of theories are being put forward:
Infectious. It is based on the fact that ulcerative colitis of the intestine is caused by a virus or a bacterium. The exact strain, however, is unknown.
Genetic. It says that ulcerative colitis is an autoimmune disease in which cells secrete antibodies that destroy epithelial cells of the intestinal mucosa (similar to how antibodies produced against iodine-containing substances destroy thyroid cells in Hashimoto’s autoimmune thyroiditis).
Hereditary. According to this theory, ulcerative colitis is inherited and is caused by aggressive environmental factors that affected the parents.
The disease is caused by the following triggers:
Hypodynamia (inactivity);
A diet rich in carbohydrates;
Lack of fiber in the diet;
stress;
Dysbacteriosis.
The disease occurs in three main forms: mild, moderate and severe.
With a mild degree of damage, the intestinal walls do not undergo serious ulceration. The disease practically does not make itself felt, except for small streaks of mucus and blood in the stool. Symptoms specific to colitis may be absent altogether.
The average degree of the course of the pathology is characterized by an increase in body temperature (up to a maximum of 38.1), cramping pain and general malaise. The urge to defecate occurs 4-6 times a day, mainly at night.
A severe degree occurs at a high temperature (over 38.1) against the background of disorders of the cardiovascular system (tachycardia). There is pallor of the skin, uneven breathing. Pain in the abdomen is strong, cramping. Urges at least 7-10 times a day. Pain especially pronounced immediately before the act.
In especially severe cases, intestinal perforation may develop, followed by sepsis, peritonitis, and massive bleeding.
Spastic colitis of the intestine
Spastic colitis differs from other types of this pathology in a significantly reduced function of the colon due to insufficient peristalsis. Unlike ulcerative colitis, spastic severe pathology is not considered and rather refers to a disorder of bowel functions.
Normally, defecation occurs with a certain frequency. For some, the norm is 1 time per day, for others – 1 time per week. In spastic colitis, the main symptom is persistent constipation. The severity of the course of the disease is still purely individual and in two patients the symptoms will be completely different.
Symptoms, in general, are similar to other forms and include:
heaviness in the abdomen, bloating;
aching pain in the left side or lower left;
A sharp alternation of constipation and diarrhea with a predominance of the latter;
Constipation persists most of the time;
increased production of gases.
Spastic intestinal colitis is easier, because the condition of patients can be described as satisfactory.
When palpation of the colon, as well as ultrasound diagnostics, spasmodic areas of the colon are clearly visible. This type of disease is characterized by changes in the intestines. In some areas, it is excessively expanded, in others, on the contrary, it is narrowed.
Prolonged disease causes gradual atrophic changes in the smooth muscles of the colon, caused by a decrease in work. The tone of the intestine falls, along the entire length of the organ, mucus secretion and swelling are observed. These signs are found during sigmoidoscopy. If degenerative or atrophic processes are detected, a more thorough diagnosis is necessary, since in this case the intestinal walls become dry and begin to crack. Fissures can be mistaken for ulcers that distinguish ulcerative colitis.
For this reason, it is important to take into account the complex of symptoms and factors in conjunction with the data of instrumental diagnostics for an accurate diagnosis.
catarrhal colitis of the intestine
Catarrhal colitis is rather not an independent type of this pathology, but a stage in its development. Catarrhal colitis is the initial stage in the formation of the pathological process. In terms of duration, the catarrhal type proceeds in 2-3 days for a period and is characterized by severe symptoms.
In addition, catarrhal colitis may not be the beginning of the disease, but only a manifestation (for example, food poisoning), which, with proper treatment, will come to naught and will not turn into a chronic form.
Symptoms of this type of colitis:
The gradual inflammation of the intestinal mucosa causes a growing feeling of discomfort in the iliac region, in the left lower abdomen or in the pubic region.
The inflamed intestine increases in size, and therefore the patient feels a strong heaviness and bloating.
A large amount of spotting is found in the stool, which indicates the process of degeneration of the mucosa.
Damaged areas undergo necrosis, therefore, even at the end of the acute phase of intestinal dysfunction, as well as pain will persist.
Catarrhal colitis, like any other type, is characterized by general manifestations, such as symptoms of intoxication (weakness, headache, irritability and fatigue, drowsiness, etc.), constipation or diarrhea, frequent tenesmus, pain, etc.
Catarrhal colitis is easy to identify even for a non-specialist without medical training, therefore, special diagnostic manipulations, in addition to taking an anamnesis, are not required to make a general diagnosis. You should carefully consider the treatment of the catarrhal type of pathology, since it is prone to rapid progression and after 8-10 days it turns into a fibrinous type, and after another week and a half it can begin to turn into an ulcerative type.
Atrophic colitis of the intestine
Atrophic colitis often goes hand in hand with spastic colitis and develops in later stages. The essence of the pathological process lies in the atrophy of the smooth muscles of the colon due to a long stagnant process. An important point should be noted. While other types of intestinal colitis affect both the large and small intestines, atrophic colitis occurs only in the large intestine.
Often, gastritis is diagnosed along with atrophic colitis, but it is not known if there is a causal relationship between these diseases.
Symptoms are similar to other types and have no special manifestations. Over time, atrophic colitis can turn into an ulcerative form, since the mucous membrane of the colon becomes thinner over time, and the number of pathological microorganisms in the organ does not decrease, which can lead to rapid degeneration of the epithelial tissue. In especially advanced cases, everything can end with perforation of the colon and severe complications, such as sepsis or severe bleeding.
The complexity of this disease lies in the complexity of diagnostic measures. Only a competent and attentive medical specialist is able to correctly differentiate the diagnosis.
Erosive colitis of the intestine

Erosive colitis is not always distinguished by specialists as a separate type. It would be more correct to speak of this type as the initial stage of development of ulcerative colitis. The only and main difference is that erosive changes are minor and do not end in perforation, however, the symptoms are characteristic enough to distinguish erosive colitis without much difficulty.
Almost always, regardless of the individual characteristics of the body, erosive colitis is represented by the whole complex of typical manifestations, including:
Nausea (the patient is sick), vomiting is possible.
Heaviness in the abdomen (located mainly in the stomach).
Pain in the stomach. An inexperienced doctor, because of this symptom, can take erosive colitis for one of the forms of gastritis and prescribe a fundamentally wrong treatment.
Sound in the abdomen (rumbling).
Metallic sour taste in mouth.
Belching and heartburn (also commonly associated with gastritis with high acidity).
Appetite disorders.
In addition to the complex of symptoms that accompany erosive colitis, the disease is also accompanied by symptoms typical of any colitis, such as stool disorders, etc.
Diffuse colitis of the intestine
Diffuse colitis of the intestine most often affects both departments at once, proceeding heavily. Because colitis affects both the large and small intestines, symptoms are prominent from day one. The symptoms include both signs of gastritis and signs of enteritis.
Diagnosing diffuse colitis is usually not that difficult with minimal medical training.
This type of pathology is characterized by a number of symptoms:
Pain sensations. Pain in the diffuse type of colitis is not localized in any one area, but spreads throughout the abdomen. Often there is a transfer of discomfort from one part of the abdomen to another (wandering pain). In some cases, on the second or third day, the pain becomes distinct and is located in the lower left or lower right side of the abdomen. In the latter case, functional tests for appendicitis should be additionally performed. The pains are aching or dull, colicky in nature.
The pain may radiate to the region of the heart. Together with a heartbeat, this gives the patient reason to assume pathologies of the heart, and not the gastrointestinal tract.
Often, when a diffuse type is detected, it is not a decrease in appetite, but its complete absence.
Very frequent tenesmus. On the first day – copious diarrhea with characteristic impurities. After the act of defecation, pain intensifies, but not immediately, but after 1.5-2 hours. The diarrhea continues for 2-3 days. A small amount of liquid with an extremely unpleasant odor of feces is allocated. Almost always, diarrhea begins at night, usually at 5-7 in the morning (the so-called “diarrhea-alarm clock”).
Nausea, vomiting. The urge to vomit persists even with an empty stomach.
Heartburn, belching.
The clinical picture is inconsistent. On x-ray examination with a contrast agent, both areas of narrowing and pathological expansion of the intestine are visible. Peristalsis can either accelerate at times or be depressed.
The patient’s tongue is coated with a gray or yellowish coating.
On palpation, hard, spasmodic areas are noted; on palpation, patients indicate pain.
Consequences of intestinal colitis
Intestinal colitis, despite seemingly frivolous manifestations, as well as the relative ease of treatment, can cause formidable complications. Acute colitis, as it was said, in the absence of proper therapy in 90% of cases turns into a chronic incurable form and haunts the patient throughout his life.
In adults, both acute and chronic colitis can cause four serious consequences:
Ulcer.
Internal bleeding.
Peritonitis.
Blood poisoning (sepsis).
Ulcers are formed mainly with an old form of chronic colitis, when an aggressive agent constantly acts on the intestinal mucosa. Ulcers can lead to perforation of the wall and the release of intestinal contents beyond its borders.
As a result of perforation, profuse internal bleeding rapidly develops, requiring immediate surgical intervention. Without medical attention, the patient risks dying from blood loss. In addition, as a result of perforation, the contents of the intestine are in the abdominal cavity and cause an infectious infection, which can also lead to death.
Sepsis. The intestine has a developed and complex circulatory system, therefore any damage to the walls of the organ entails damage to the blood vessels at the same time. Fecal masses are rich in harmful substances and pathogenic organisms, which, once in the blood, can cause its infection. The risk of sepsis is especially high with an infectious cause of intestinal colitis.
In addition, colitis, especially chronic, is always accompanied by stagnant processes in the large intestine. As a result, harmful substances are not removed from the body in time and are absorbed back into the blood, poisoning the body. In patients, signs of intoxication are constantly observed: weakness, headache, appetite disorders, etc.
Also, colitis can lead to dehydration of the body, since most of the water does not have time to be absorbed in the large intestine and comes out with frequent diarrhea.
A fairly common and dangerous consequence of colitis is intestinal obstruction. Since the peristalsis of the intestine weakens, the feces are not evacuated from the body and acquire a stony structure. Gradually accumulating, they are able to cause complete closure of the intestinal lumen. In this case, surgical intervention in the shortest possible time is indispensable.
Differential diagnosis of intestinal colitis
Modern medicine has a wide range of laboratory and instrumental research methods. With their help, you can determine the presence of pathology, its stage and form.
Laboratory methods
Laboratory methods for the differential diagnosis of colitis include:
General blood analysis. The clinical picture of intestinal colitis is characterized by an inflammatory process, which means that a high erythrocyte sedimentation rate (ESR), a significant concentration of platelets, leukocytosis, and a low level of hemoglobin will be determined in the blood.
Fecal analysis (coprogram). In the feces, the content of blood, leukocytes and erythrocytes can be observed.
Stool cultures for infectious and bacterial agents (dysentery, cholera, tuberculosis, etc.).
PCR diagnostics. Allows you to identify helminthiasis, as well as viral lesions of the intestine.
Analysis for the presence of specific antibodies to the cytoplasm of neutrophil cells (pANCA) allows you to determine the presence of genetic autoimmune pathologies that reduce the efficiency of the intestine.
Analysis for fecal calprotectin. It is carried out in order to identify Crohn’s disease, a secondary symptom of which may be colitis.
Instrumental methods
Instrumental methods for the differential diagnosis of colitis include:
Contrast irrigoscopy. During the study, a contrast agent is injected into the rectum of the patient. After some time, an x-ray is performed, which allows to assess the degree of functional disorders of the organ. Irrigoscopy makes it possible to exclude the growth of tumors, stenosis of the intestinal walls, etc.
Fibroileocolonoscopy. Endoscopic examination of the intestine. Allows you to determine the location of the pathological process, its nature and stage, as well as take biological material for research (to exclude malignant neoplasms and the possibility of their formation).
Ultrasonography. It is carried out in order to identify changes in the lumen of the intestine or the walls of the organ.
MRI
Examination by a proctologist with a digital examination of the anus and rectum. It is carried out in order to exclude pathologies of the rectum: paraproctitis, as well as anal fissures and hemorrhoids.
Ultrasound examination Abdominal organs and liver function tests reveal inflammation of the liver, pancreas, and gallbladder.
Biopsy. The symptoms and clinical picture of colitis are very similar to those of various malignant neoplasms. Suspicious intestinal fragments should be biopsied to rule out cancer.
How to treat intestinal colitis?

In order to prescribe treatment or recognize colitis, you must consult a gastroenterologist or a coloproctologist. The main link in the chain of treatment of colitis is a special diet.
Diet
The treatment of colitis, unlike the treatment of many other diseases, is characterized by the fact that diet is an integral element of therapy. Since the mucous membrane of the large (and possibly small) intestine is irritated, in no case should it be irritated even more. Therefore, the goal of the diet is to minimize the burden on the intestines, while maintaining an optimal diet rich in everything you need.
Foods rich in fiber are temporarily excluded from the diet:
sunflower seeds, pumpkin seeds
Peanut
Raw fruits and vegetables
Bran
Marinade and smoked meats
All salty, sour and sweet foods
Food should be soft, therefore, during heat treatment, preference is given to steaming, boiling.
Nutrition should be fractional, 4-6 times a day, to avoid unnecessary stress on the digestive tract. Products that improve intestinal motility and have a laxative effect should also not be eaten. This applies to prunes, milk, pumpkin, cabbage, etc. It is best to eat pureed food.
With colitis, you should drink enough fluids, as the body quickly dehydrates.
Methods of medical treatment
We also list a number of measures that can be applied during treatment:
Antibiotics and antimicrobials. They are prescribed if an infectious etiology of the disease is detected. The course of treatment is 3-5 days strictly according to the indications and under the supervision of the attending physician.
Helminthiasis. If the cause of intestinal colitis is helminthiasis (a parasitic lesion of the intestine), specialized anthelmintic drugs are prescribed (specific names depend on the type of helminth and the degree of damage).
Removal of pain syndrome. A pronounced pain syndrome is removed with antispasmodic drugs. In more severe cases, anticholinergic drugs are added to antispasmodics.
Treatment of associated complications. With colitis of the intestine, proctitis or proctosigmoiditis is often formed. To eliminate these consequences of colitis, specific local therapy is carried out using suppositories, as well as enemas.
Elimination of stool disorders. Constipation and diarrhea are eliminated in various ways. Astringents are recommended to stop diarrhea, a cleansing enema is performed to eliminate constipation, and laxatives are taken.
Normalization of microflora. Normal and stable peristalsis is impossible without beneficial microflora. As a result of diarrhea or constipation, the microflora dies. If cleansing measures were taken, the bacteria are washed out, as a result of which prolonged constipation may begin. Special preparations-probiotics, enterosorbents are prescribed.









