Contents

Hemotransfusion is a blood transfusion procedure that has certain indications, can cause complications, and therefore requires preliminary preparation.
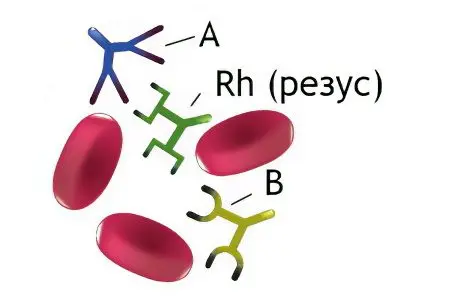
The first attempts to transfuse blood to a person were made long before the birth of Christ. At that time, people tried to introduce the blood of animals: lambs, dogs, pigs, which, of course, was not successful. Then, experimentally, it was found that only human blood is suitable for a person. People learned about blood compatibility only in 1901, when the scientist Karl Landsteiner discovered the antigenic blood system ABO (blood groups). This was a real breakthrough in medicine, which made it possible to perform blood transfusion from person to person without more or less dangerous health consequences. Even 40 years later, the Rhesus system was discovered, which made this procedure even more accessible.
What is a blood transfusion?
Blood for transfusion is taken from people voluntarily. This is carried out in medical institutions, blood banks and blood transfusion stations. Blood taken from a donor is stored in containers so that it does not deteriorate, special preservatives and stabilizers are added to it. Without fail, blood is examined for various infectious diseases, such as: HIV, gonorrhea, hepatitis. Various components are also extracted from the blood: red blood cells, plasma, platelets. Medicines are made from blood: gamma globulin, albumin, cryoprecipitate, etc.
The procedure for a blood transfusion is similar to the procedure for transplanting tissue from one person to another. It is simply impossible to find blood that is ideal in all respects, so whole blood is rarely transfused. This happens only when the patient needs an emergency direct blood transfusion. In order for the body to give a minimum of side effects, the blood is divided into components. Most often they are erythrocytes and plasma.
To prevent a person from becoming infected with dangerous infectious diseases, such as HIV or hepatitis, blood taken from a donor is sent to quarantine, where it is stored for 6 months. Ordinary refrigerators are not suitable for this, since under such conditions the blood will lose its beneficial properties. So, platelets are stored for 6 hours, red blood cells can exist for no more than 3 weeks in the refrigerator, but after freezing they are destroyed. Therefore, blood received from a donor is divided into red blood cells, which can be frozen at -196 °C using nitrogen. Blood plasma can also withstand ultra-low temperatures. The process of blood storage is very complex and requires a selective approach.

Most people who, due to their professional activities, are not related to medicine, know only about the most common method of blood transfusion. In this case, blood from a container (vial or gemakon – a bag with blood and a preservative) is fed through a puncture in a vein into the patient’s bloodstream. Preliminary, the patient’s blood is examined to determine its group and Rh factor, if this is not known. Then he is injected with the blood that suits the person in all respects.
If earlier it was believed that any blood is suitable for a person, the main thing is that it be obtained from a person, then modern medicine does not share this point of view. A compatibility test is required first.
Blood can be transfused from a donor to a recipient for the following purposes:
The function of replacing one’s own blood.
hemostatic function.
stimulating function.
Removal of intoxication.
nutritional function.
Carrying out blood transfusion requires a careful attitude on the part of the doctor. The procedure should be performed only if there are certain indications for it. Unjustified blood transfusion threatens with serious health problems, because only identical twins can have 100% blood compatibility. In other people, even though they are blood relatives, the blood differs in a number of individual indicators. Therefore, there is no guarantee that the body will not begin to reject it.
Ways and methods of blood transfusion

There are several ways of blood transfusion, each of which is designed to solve certain goals and objectives.
Among those:
Indirect transfusion, when the patient is transfused with donated blood stored in certain containers.
Direct blood transfusion, when the patient is transfused with blood immediately from the donor’s vein. This procedure is carried out using special equipment. The device makes it possible to perform continuous blood transfusion, and with the help of a syringe, intermittent transfusion is performed.
Exchange transfusion, when the patient is transfused with blood after his blood has been partially or completely removed.
Autohemotransfusion. In this case, the patient is transfused with pre-prepared donor blood during the operation. In this case, the donor and the patient are one and the same person.
Reinfusion. At the same time, a person’s own blood, which was poured out during an accident or during an operation, is collected and then transfused to the person himself.
Blood is transfused drip, jet or jet-drip. The doctor should decide on the speed of the transfusion.
Blood transfusion is a complex procedure that is compared to surgery, so its implementation is the responsibility of the doctor, and not the junior medical staff.
Methods of blood supply to the recipient:
Intravenous infusion is the basic method of blood transfusion. Venepuncture is a standard blood transfusion, and venesection is a method of transfusing blood through a catheter that is placed in the subclavian vein. The device can be in this place for a long time, but the catheter must be properly cared for.
Intra-arterial blood transfusion is performed very rarely when a person has a cardiac arrest.
It is possible to perform intraosseous blood transfusion. For this purpose, the bones of the sternum and ilium are most often used. Less commonly, blood is injected into the calcaneus, into the condyles of the femur, and into the tuberosity of the tibia.
Intracardiac blood transfusion is carried out in the left ventricle. This method of blood transfusion is implemented in practice extremely rarely, when other methods are not available.
An intra-aortic transfusion may be performed when there are only a few seconds to save a person’s life. Indications can be: unexpected clinical death, massive blood loss during surgery in the sternum.
It is important to distinguish between autohemotransfusion and autohemotherapy, as these are two radically different procedures. With autohemotransfusion, a person is given a full transfusion of his own blood, which was previously harvested. With autohemotherapy, the patient’s own blood is transfused from a vein into the buttock. This procedure is aimed at eliminating cosmetic defects, such as youthful acne, pustular skin lesions, etc.
Preparing for a blood transfusion
Blood transfusion requires careful preparation of the person. First of all, this concerns the qualitative collection of anamnesis, as well as the study of the patient’s allergic tension.
Therefore, the doctor must ask the patient the following questions:
Has he had a blood transfusion before? If so, how did he endure this procedure?
Does the person suffer from allergies?
The woman finds out how many births she had, whether they all ended successfully. If the patient has a aggravated history, then additional examinations are indicated for her, including: the Coombas test, which allows the detection of immune antibodies.
It is imperative to find out what diseases the patient has previously suffered, and what pathologies he suffers from at this point in time.
In general, the doctor faces the task of qualitatively examining the patient and finding out if he is at risk of people who are contraindicated in blood transfusion.
Depending on the purpose of the transfusion, the doctor may administer certain blood components to the patient. I rarely use whole blood.
Preliminary preparation is reduced to the following steps:
Determination of the patient’s blood group and the Rh factor of the blood, if he does not have a written certificate with a seal confirming these indicators.
Determination of the blood type and Rh factor of the donor, despite the fact that such a mark is already on the blood vial.
Performing a biological test for the compatibility of the blood of the donor and the recipient.
Sometimes an emergency blood transfusion is required, in which case all the preparatory steps are carried out at the discretion of the doctor. If surgical intervention is planned, then the patient must adhere to a diet for several days, cutting back on protein foods in his diet. On the day of surgery, only a light breakfast is allowed. If the intervention is scheduled for the morning, then the patient’s intestines and bladder should be empty.
Indications and contraindications for blood transfusion

Even despite the fact that the preparation for the process of blood transfusion is carried out according to all the rules, this procedure still provokes sensitization of the body. Moreover, there is always the risk of immunizing the body with antigens that modern medicine does not yet know about. Therefore, there are practically no indications for whole blood transfusion.
The only exceptions are the following situations:
Acute loss of blood by a person when its total volume is about 15% of the total circulating blood volume.
Bleeding against the background of a violation of the hemostasis system. If possible, the patient is transfused not with whole blood, but with the necessary elements.
Shock condition.
Severe anemia.
Injury or complex operation, which is accompanied by massive blood loss.
Hemotransfusion with whole blood has much more contraindications to its implementation than indications. The main contraindication is a wide variety of diseases of the cardiovascular system. However, when it comes to transfusion of red blood cells or other individual blood elements, absolute contraindications often become relative.
So, absolute contraindications to whole blood transfusion include:
Septic endocarditis in subacute and acute stages.
thrombosis and embolism.
Disturbances of cerebral circulation of the expressed intensity.
Pulmonary edema.
Myocarditis and myocardiosclerosis.
The third stage of arterial hypertension.
Third and 2B degree of circulatory disorders.
Atherosclerosis of cerebral vessels.
Nephrosclerosis.
Hemorrhages in the retina.
Rheumatism in the acute stage, rheumatic fever.
Renal and liver failure in acute and chronic stages.
Relative contraindications:
Amyloidosis.
Disseminated pulmonary tuberculosis.
Hypersensitivity to proteins and protein preparations.
Allergy.
If a situation is created that poses a direct threat to human life, then absolute contraindications are not paid attention to. After all, there are cases when, without a speedy blood transfusion, a person simply dies. However, even then it is highly desirable to transfuse the patient not with whole blood, but with its individual components, for example, red blood cells. Doctors also try to replace the blood with special solutions as much as possible. In parallel, the patient is shown the introduction of antiallergic drugs.
Blood for transfusion and its components
Human blood is made up of blood cells and plasma. Various preparations are prepared from these components, although this process cannot be called technologically easy.
The most common blood components extracted from whole blood are leukocytes, plasma, platelets and red blood cells.
Erythrocytes
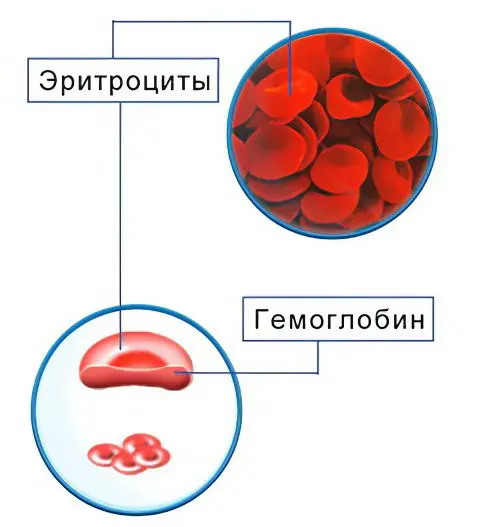
Erythrocytes are transfused when there is a shortage of red blood cells. Indications for the procedure are hematocrit below 0,25 and hemoglobin below 70 g/l.
This can happen under the following conditions:
Anemia developing in the early postpartum period, or in the early postoperative period.
Severe iron deficiency anemia, which develops in older people due to heart or respiratory failure, or in young women during childbearing. The procedure in this case can be carried out before the onset of childbirth or before the upcoming operation.
Anemia on the background of various diseases of the digestive system.
Intoxication of the body against the background of severe burns, poisoning, purulent processes. Erythrocytes from the donor’s blood allow the patient’s body to be rid of toxic substances.
Erythropoiesis, which caused anemia.
If the patient has symptoms that indicate a violation of blood microcirculation, then he is transfused with an erythrocyte suspension. It is a dilute mass of red blood cells.
To minimize the risk of developing adverse reactions from the body, it is necessary to use washed erythrocytes three times or five times for transfusion. With the help of saline, platelets, leukocytes, preservatives, electrolytes, microaggregates and other substances that the body of a sick person does not need are removed from them. If the erythrocyte mass has been subjected to the procedure for removing leukocytes and platelets from it, then it is called EMOL.
The blood that is currently being used for transfusion is frozen after being taken from a donor. Therefore, they wash the erythrocyte mass on the day when they are going to perform its transfusion.
EMOLT is infused in patients according to the following indications:
If the patient has previously experienced complications caused by blood transfusion.
The presence of isoimmune or autoimmune antibodies in the patient’s blood. A similar situation is often observed in hemolytic anemia.
Washing of erythrocytes is required when it is necessary to transfuse a large amount of blood, which reduces the risk of developing the syndrome of massive blood transfusions.
Increased blood clotting.
The patient has renal or hepatic insufficiency.
Thus, it becomes obvious that EMOLT makes it possible to help a person who has absolute contraindications to whole blood transfusion.
Plasma

Plasma contains a large amount of protein components, vitamins, antibodies, hormones and other useful substances that are required by patients in a wide variety of situations. Therefore, plasma is a component of blood, which is in great demand for transfusion. It can also be used in combination with other blood components.
Plasma is transfused in the following cases: a decrease in the total volume of circulating blood, bleeding, immunodeficiency, exhaustion and other serious health problems.
Platelets

Platelets are plates that take part in the process of hematopoiesis. They form white blood clots, necessary to stop bleeding from the capillaries. The fewer platelets in the human body, the higher the risk of bleeding. If their level drops to a critical zero level, then the likelihood of hemorrhage in the brain increases.
The storage and harvesting of platelets is a very complex process. The platelet mass cannot be prepared in advance at all, since it is stored for a very short time, and also requires constant mixing. Therefore, platelets are transfused only on the day of collection from the donor. Before this, the blood is urgently checked for infections.
Most often, a person who is a relative of the victim acts as a donor. Alloimmunization develops in those patients who often receive platelet transfusions. Also, this condition is a frequent companion of women who have undergone a difficult abortion or childbirth, as a result of which they needed donor blood.
In order for platelet transfusion to be successful, it is highly desirable to conduct an analysis for the selection of platelets according to the antigens of the HLA leukocyte system. This analysis is very costly financially and also very time consuming.
In addition, platelet transfusion is associated with the risk of developing another reaction, which is called “graft-versus-host”. This happens when aggressive T- and B-cells are present in the donor’s platelets. Therefore, transfusion of platelets is quite a challenge.
Indications for platelet transfusion:
Thrombocytopathies, which are accompanied by increased bleeding. This pathology can be either acquired or congenital. If the platelet level reaches 60,0 * 109/l, but there is no hemorrhagic syndrome, then this is not an indication for blood transfusion. The platelet mass is transfused when the platelet level reaches 40 * 109/ L.
Surgical intervention.
Preparation for treatment with cytostatics.
leukocytes
WBC transfusion is an even more complex task than platelet transfusion. This procedure is carried out for the treatment of leukopenia, and it is also indicated for patients who have undergone radiation or chemotherapy.
Often this procedure is abandoned, since it is very difficult to obtain a high-quality leukocyte mass. It is mined only with the use of a separator. After removal from the donor’s body, leukocytes die very quickly. In addition, the transfusion of leukocyte mass is associated with complications such as chills, shortness of breath, tachycardia, fever, and a drop in blood pressure.
Hemotransfusion to a newborn baby
Indications for blood transfusion in a newborn child are similar to those for blood transfusion in an adult. The selection of the blood dose is carried out on an individual basis. Doctors should be especially attentive to children who were born with hemolytic disease of the newborn.
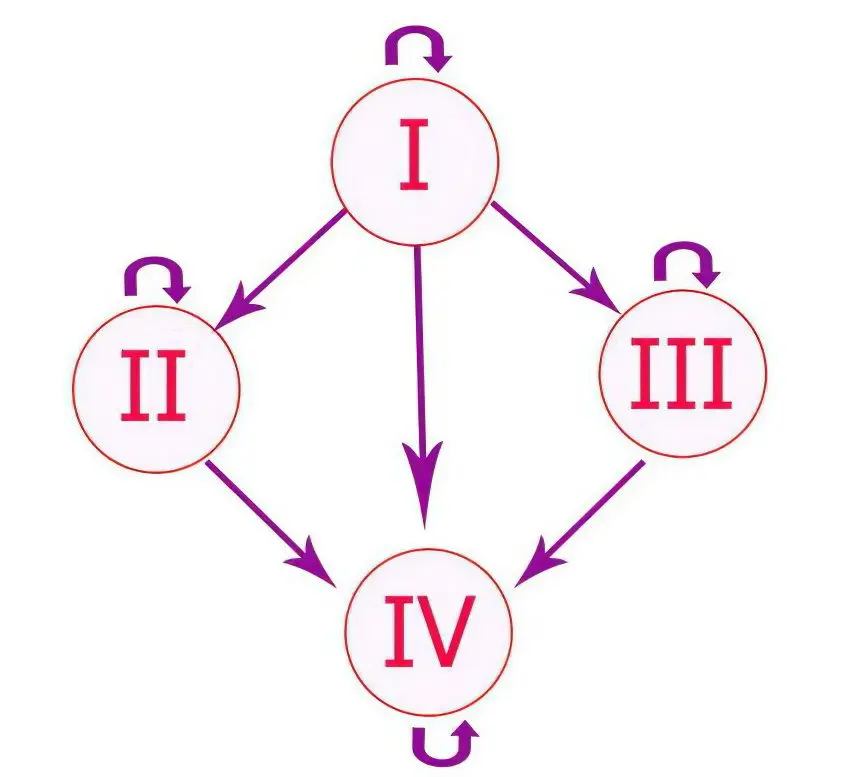
In case of hemolytic jaundice, the child undergoes an exchange blood transfusion using an EMLT of group 0 (I), with a mandatory match of the Rh factor.
Transfusion of blood to a newborn child is a complex process that requires caution and utmost attention from the doctor.
Complications from a blood transfusion
Complications during blood transfusion most often develop due to the fact that medical personnel made errors in storage, blood preparation or during the procedure.
The main reasons that can lead to complications include:
Incompatibility of the donor and the patient by blood type. In this case, transfusion shock develops.
The patient is allergic to immunoglobulins contained in the donor’s blood.
Poor quality blood from a donor. In this case, the development of potassium intoxication, bacterial toxic shock, pyrogenic reactions is possible.
Mass blood transfusion, which can provoke homologous blood syndrome, acute dilated heart, massive transfusion syndrome, citrate intoxication.
Transmission of infection along with the blood of a donor. Although its long-term storage reduces this complication to a minimum.
Destruction (hemolysis) of foreign red blood cells:
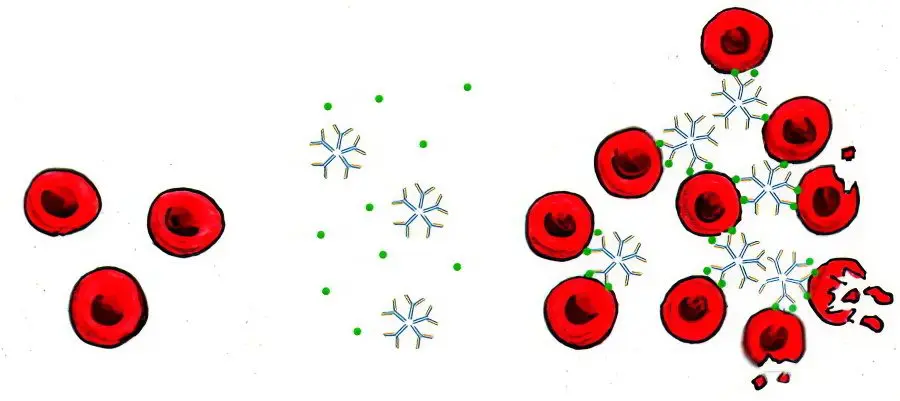
If the patient develops one or another negative reaction, the doctor must take emergency measures. Symptoms of such complications will be obvious: a person’s body temperature rises, chills increase, and suffocation may develop. The skin turns blue, blood pressure drops sharply. Every minute a person’s condition will worsen, up to the development of acute renal failure, pulmonary embolism, pulmonary infarction, etc.
Any mistake made by the medical staff during the blood transfusion process can cost a person a life, so you need to approach the procedure as responsibly as possible. It is unacceptable for a blood transfusion to be performed by a person who does not have sufficient knowledge about this procedure. In addition, blood transfusion should be carried out exclusively under strict indications.
Report on blood donation and transfusion:









