Contents
What is autoimmune hepatitis?

Autoimmune Hepatitis (AIH) is a progressive liver lesion of an inflammatory-necrotic nature, in which the presence of liver-oriented antibodies in the blood serum and an increased content of immunoglobulins are detected. That is, with autoimmune hepatitis, the liver is destroyed by the body’s own immune system. The etiology of the disease has not been fully elucidated.
The direct consequences of this rapidly progressive disease are kidney failure and cirrhosis of the liver, which can eventually lead to death.
According to statistics, autoimmune hepatitis is diagnosed in 10-20% of cases of the total number of all chronic hepatitis and is considered a rare disease. Women suffer from it 8 times more often than men, while the peak incidence occurs in two age periods: 20-30 years and after 55 years.
Causes of autoimmune hepatitis
The causes of autoimmune hepatitis are not well understood. The fundamental point is the presence of a deficiency of immunoregulation – the loss of tolerance to one’s own antigens. It is assumed that a certain role is played by hereditary predisposition. Perhaps such a reaction of the body is a response to the introduction of some infectious agent from the external environment, the activity of which plays the role of a “trigger” in the development of the autoimmune process.
Measles, herpes (Epstein-Barr) viruses, hepatitis A, B, C and some medications (Interferon, etc.) can act as such factors.
Diseases associated with AIH:
Autoimmune thyroiditis;
Graves’ disease;
Vitiligo;
Hemolytic and pernicious anemia;
Herpetiform dermatitis;
Gingivitis;
Glomerulonephritis;
insulin-dependent diabetes mellitus;
Iritis;
Lichen planus;
Local myositis;
Neutropenic fever;
Nonspecific ulcerative colitis;
Pericarditis, myocarditis;
Neuropathy of peripheral nerves;
Pleurisy;
Primary sclerosing cholangitis;
Rheumatoid arthritis;
Cushing’s syndrome;
Sjogren’s syndrome;
Synovitis;
Systemic lupus erythematosus;
erythema nodosum;
fibrosing alveolitis;
Chronic urticaria.
Of these, the most common in combination with AIH are rheumatoid arthritis, ulcerative colitis, synovitis, and Graves’ disease.
Types of autoimmune hepatitis
Depending on the antibodies detected in the blood, 3 types of autoimmune hepatitis are distinguished, each of which has its own characteristics of the course, a specific response to therapy with immunosuppressive drugs and prognosis.
Type 1 (anti-SMA, anti-ANA positive)
It can appear at any age, but is more often diagnosed in the period of 10-20 years and over the age of 50 years. If untreated, 43% of patients develop cirrhosis within three years. In the majority of patients, immunosuppressive therapy gives good results, stable remission after stopping the drugs is observed in 20% of patients. This type of AIH is most common in the United States and Western Europe.
Type 2 (anti-LKM-l positive)
It is observed much less frequently, accounting for 10-15% of the total number of AIH cases. Mostly children are ill (from 2 to 14 years). This form of the disease is characterized by a stronger biochemical activity, cirrhosis of the liver within three years is formed 2 times more often than with type 1 hepatitis.
Type 2 is more resistant to drug immunotherapy, and discontinuation of the drugs usually results in a relapse. More often than in type 1, there is a combination with other immune diseases (vitiligo, thyroiditis, insulin-dependent diabetes mellitus, ulcerative colitis). In the US, type 2 is diagnosed in 4% of adult patients with AIH, while type 1 is diagnosed in 80%. It should also be noted that 50-85% of patients with type 2 disease and only 11% with type 1 suffer from viral hepatitis C.
Type 3 (anti-SLA positive)
With this type of AIH, antibodies to the liver antigen (SLA) are formed. Quite often, with this type, rheumatoid factor is detected. It should be noted that 11% of patients with type 1 hepatitis also have anti-SLA, so it remains unclear whether this type of AIH is a type 1 variant or should be distinguished into a separate type.
In addition to traditional types, sometimes there are forms that, in parallel with the classical clinic, may have signs of chronic viral hepatitis, primary biliary cirrhosis, or primary sclerosing cholangitis. These forms are called cross-over autoimmune syndromes.
Symptoms of autoimmune hepatitis

In about 1/3 of cases, the disease begins suddenly, and its clinical manifestations are indistinguishable from those of acute hepatitis. Therefore, the diagnosis of viral or toxic hepatitis is sometimes erroneously diagnosed. Severe weakness appears, there is no appetite, urine becomes dark in color, intense jaundice is observed.
With the gradual development of the disease, jaundice may be insignificant, periodically there are heaviness and pain on the right under the ribs, autonomic disorders play a predominant role.
At the peak of symptoms, nausea, pruritus, lymphadenopathy (swollen lymph nodes) join the above symptoms. Pain and jaundice are intermittent, aggravated during exacerbations. Also, during exacerbations, signs of ascites (accumulation of fluid in the abdominal cavity) may appear. There is an enlargement of the liver and spleen. Against the background of autoimmune hepatitis, amenorrhea appears in 30% of women, hirsutism (increased hair growth) is possible, and gynecomastia in boys and men.
Typical skin reactions are capillaritis, erythema, telangiectasias (spider veins) on the face, neck, hands, and acne, since almost all patients have abnormalities in the endocrine system. Hemorrhagic rash leaves behind pigmentation.
The systemic manifestations of autoimmune hepatitis include polyarthritis of large joints. This disease is characterized by a combination of liver damage and immune disorders. There are diseases such as ulcerative colitis, myocarditis, thyroiditis, diabetes, glomerulonephritis.
However, in 25% of patients, the disease is asymptomatic in the early stages and is detected only at the stage of liver cirrhosis. With signs of the presence of any acute infectious process (herpes virus type 4, viral hepatitis, cytomegalovirus), the diagnosis of autoimmune hepatitis is called into question.
Diagnostics
Diagnostic criteria for the disease are serological, biochemical and histological markers. Research methods such as ultrasound, MRI of the liver do not play a significant role in terms of diagnosis.
The diagnosis of “autoimmune hepatitis” can be made under the following conditions:
There are no facts of blood transfusion, taking hepatotoxic drugs, recent alcohol consumption in the anamnesis;
The level of immunoglobulins in the blood exceeds the norm by 1,5 times or more;
No markers of active viral infections (hepatitis A, B, C, Epstein-Barr virus, cytomegalovirus) were found in the blood serum;
Antibody titers (SMA, ANA and LKM-1) exceed 1:80 for adults and 1:20 for children.
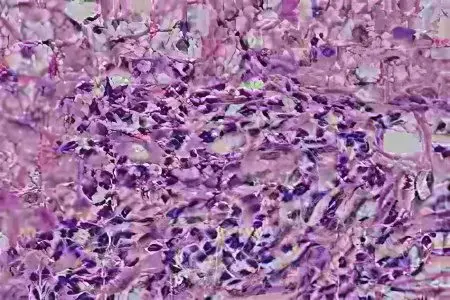
The final diagnosis is confirmed based on the results of a liver biopsy. Histological examination should reveal stepped or bridging tissue necrosis, lymphoid infiltration (accumulation of lymphocytes).
Autoimmune hepatitis must be differentiated from chronic viral hepatitis, Wilson’s disease, drug-induced and alcoholic hepatitis, non-alcoholic fatty liver disease, cholangitis, and primary biliary cirrhosis. The presence of such pathologies as damage to the bile ducts, granulomas (nodules formed against the background of the inflammatory process) is also unacceptable – most likely, this indicates some other pathology.
AIH differs from other forms of chronic hepatitis in that in this case, it is not necessary to wait for the disease to become chronic (ie, about 6 months) to make a diagnosis. AIH can be diagnosed at any time during its clinical course.
Treatment of autoimmune hepatitis

The basis of therapy is the use of glucocorticosteroids – immunosuppressive drugs (suppressing immunity). This allows you to reduce the activity of autoimmune reactions that destroy liver cells.
Currently, there are two treatment regimens: combined (prednisolone + azathioprine) and monotherapy (high doses of prednisolone). Their effectiveness is approximately the same, both schemes achieve remission and increase the survival rate. However, combination therapy is characterized by a lower incidence of side effects, which is 10%, while in the treatment of prednisone alone, this figure reaches 45%. Therefore, if azathioprine is well tolerated, the first option is preferable. Especially combination therapy is indicated for elderly women and patients suffering from diabetes, osteoporosis, obesity, increased nervous excitability.
Monotherapy is prescribed for pregnant women, patients with various neoplasms, suffering from severe forms of cytopenia (deficiency of certain types of blood cells). With a course of treatment not exceeding 18 months, pronounced side effects are not observed. During treatment, the dose of prednisolone is gradually reduced. The duration of treatment for autoimmune hepatitis ranges from 6 months to 2 years, in some cases, therapy is carried out throughout life.
Indications for steroid therapy
Treatment with steroids is mandatory prescribed for disability, as well as the detection of bridging or stepwise necrosis in the histological analysis. In all other cases, the decision is made on an individual basis. The effectiveness of treatment with corticosteroid drugs has been confirmed only in patients with an actively progressive process. With mild clinical symptoms, the benefit-risk ratio is unknown.
In case of failure of immunosuppressive therapy for four years, with frequent relapses and severe side effects, the only solution is liver transplantation.
Prognosis and prevention

If there is no treatment, then autoimmune hepatitis progresses, spontaneous remissions are impossible. The inevitable consequence is liver failure and cirrhosis of the liver. The five-year survival rate in this case is in the range of 50%.
In patients with stepwise necrosis, the incidence of cirrhosis within five years is 17%. If there are no complications such as ascites and hepatic encephalopathy, which reduce the effectiveness of steroid therapy, the inflammatory process in 15-20% of patients self-destructs, regardless of the activity of the course of the disease.
The results of liver transplantation are comparable to remission achieved with medications: 90% of patients have a favorable 5-year prognosis.
With this disease, only secondary prevention is possible, which consists in regular visits to a gastroenterologist and constant monitoring of the level of antibodies, immunoglobulins and liver enzyme activity. Patients with this disease are advised to follow a sparing diet and diet, limit physical and emotional stress, refuse preventive vaccination, and limit the intake of various medications.









