Contents
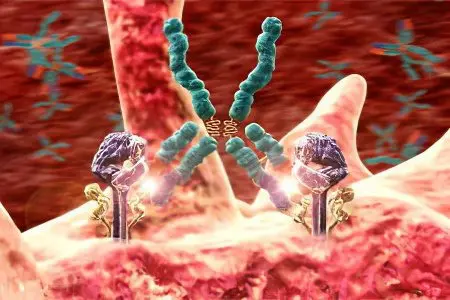
Autoimmune anemia is a disease that is characterized by increased destruction of healthy red blood cells due to the aggressive influence of antibodies on them. These antibodies are produced by the body itself. Pathology is manifested by pallor of the skin, an increase in the size of the liver and spleen, pain in the lower back and abdomen, shortness of breath and other symptoms. To detect anemia of an autoimmune nature, laboratory tests will be required. Treatment is conservative, although surgery to remove the spleen is sometimes required.
Autoimmune anemia is not very common. This disease affects one person out of 70-80 thousand. Autoimmune anemia is more often diagnosed in women, age does not matter. This type of anemia develops in both children and adults.
As a rule, the diagnosis of anemia of an autoimmune nature is not difficult. Standard blood tests make it possible to make the correct diagnosis in 90% of cases.
Full recovery is observed in no more than 50% of cases. However, an improvement in a person’s well-being during treatment with glucocorticosteroids occurs in 85-90% of cases.
Causes and pathogenesis of autoimmune anemia
Autoimmune anemia can be idiopathic (primary) or symptomatic (secondary). If the cause of the destruction of red blood cells can be established, then they speak of secondary anemia. When the etiological factor remains unclear, the anemia is called idiopathic.
The reasons for the development of autoimmune anemia (secondary) are:
Lymphoblastic leukemia of acute or chronic course.
Effects of radiation on the human body.
The presence of a malignant tumor in the body.
Connective tissue diseases, including: systemic lupus erythematosus, rheumatic fever, systemic scleroderma, etc.
Past infections, such as mycoplasmosis and cytomegalovirus infection.
Autoimmune diseases not associated with damage to the hematopoietic system, for example, thyroiditis, Crohn’s disease, sarcoidosis, etc.
Diabetes mellitus of the first type.
Treatment with antibiotics from the group of cephalosporins or penicillins.
immunodeficiency states.
More often than others, the thermal form of autoimmune anemia occurs, when the internal environment of the body has normal temperature values, and class G immunoglobulins, as well as components C3 and C4, are located on erythrocytes. The destruction of red blood cells occurs only in the spleen with the participation of macrophages.
The cold form of autoimmune anemia may have an unknown cause, or develop against the background of infection (with mononucleosis or mycoplasmal pneumonia), against the background of hypothermia, and with lymphoproliferative diseases. In the latter case, people over 60 suffer. A pathological reaction in the body, accompanied by the destruction of red blood cells, manifests itself after the temperature in the peripheral vessels drops to 32 ° C or less. Cold autoagglutinins are class M immunoglobulins.
Hemolysis occurring in the spleen is often very severe. And sometimes it is not possible to save the patient.
The course of anemia provoked by infections is most often acute. If the violation was caused by an unknown cause, then it becomes chronic.
A rare form of autoimmune anemia is paroxysmal cold anemia. In this case, hemolysis develops when the body is exposed to cold. Even drinking cold drinks and washing hands in cool water is dangerous. Sometimes such anemia is diagnosed against the background of syphilis. The severity of the course of the disease varies from case to case. Sometimes an incurable form of pathology can be observed, leading to death.
Symptoms of autoimmune anemia

Autoimmune anemia is characterized by two syndromes: anemic and hemolytic.
The following signs indicate the development of an anemic syndrome:
Pale skin and mucous membranes.
Attacks of dizziness.
Frequent nausea.
Increased heart rate.
Weakness that occurs regardless of the degree of physical or mental stress on a person.
Increased fatigue.
Hemolytic syndrome is expressed by the following symptoms:
Depending on the intensity of hemolysis, the skin may become light yellow or dark yellow.
The spleen increases in size, in the left hypochondrium painful sensations begin to disturb.
Urine turns brown.
It is possible to develop DIC with the formation of multiple blood clots and bleeding that is difficult to stop.
Acute anemia most often develops against the background of an infectious infection of the body. Therefore, in addition to signs of destruction of red blood cells, a person will have symptoms of the underlying disease.
Cold autoimmune anemia is characterized by a chronic course. When a person is exposed to low temperatures, he has blanching of the fingers and toes, auricles, face, as well as thrombophlebitis. Ulcers and even gangrene can form. Sometimes patients note the development of cold urticaria. Skin lesions persist for a long period of time.
Heat anemia also has a chronic course. The exacerbation of the pathological process occurs against the background of an increase in body temperature, which is often observed in viral and bacterial infections. A characteristic feature is the staining of urine in black.
Acute autoimmune anemia is characterized by fever, chills, headaches, and dizziness. In parallel, shortness of breath joins, there are pains in the abdomen and in the lumbar region. The skin turns pale, may become yellow, subcutaneous hemorrhages appear on the limbs. In addition to the spleen, the liver increases in size.
In the chronic course of the pathological process, a person feels satisfactory. An enlargement of the spleen in size and recurrent jaundice may indicate an existing violation. Attacks of remission alternate with attacks of exacerbation.
Diagnosis of autoimmune anemia

To make a correct diagnosis, an external examination of the patient is not enough. In addition to collecting anamnesis, blood donation will be required. A blood test indicates an increase in ESR, reticulocytosis, normo- or hypochromic anemia, and an increase in the level of bilirubin in the blood are also detected. At the same time, the level of hemoglobin and red blood cells decreases.
You need to take a urine test. It will reveal protein, an excess amount of hemoglobin and urobilin.
The patient is also referred for an ultrasound of the internal organs with a study of the state of the liver and spleen.
If the data obtained is not enough to make a correct diagnosis, then a bone marrow sampling is necessary, for which its puncture is performed. After examining the material obtained, it will be possible to detect hyperplasia of brain tissues, which occurs due to the activation of erythropoiesis. A similar goal as bone marrow puncture is pursued by a diagnostic procedure called trepanobiopsy. However, it is more difficult to tolerate by patients, so it is rarely used.
A direct Coombs test for autoimmune anemia will be positive. However, when negative test results are obtained, autoimmune anemia cannot be ruled out. This is often observed against the background of treatment with hormonal drugs or with too intense hemolysis.
ELISA allows you to identify the class and type of immunoglobulins that are involved in the autoimmune reaction.
Treatment of autoimmune anemia

Treatment of anemia of an autoimmune nature is most often long-term and does not always end with a complete recovery of the patient. First you need to decide on the reasons that led to the fact that the body began to destroy its own red blood cells. If the etiological factor can be identified, then efforts should be directed to its elimination.
If the cause remains unidentified, that is, the diagnosis sounds like “idiopathic autoimmune anemia”, then the patient is prescribed drugs from the group of glucocorticosteroids. The drug of choice is Prednisolone. If the course of anemia is severe and the level of hemoglobin in the blood drops to 50 g / l, then it is impossible to do without red blood cell transfusion.
Blood detoxification is performed in order to remove the decay products of red blood cells from it and improve a person’s well-being. Plasmapheresis makes it possible to reduce the level of antibodies that circulate in the bloodstream. Symptomatic treatment is mandatory. To prevent the development of DIC, the patient is prescribed indirect anticoagulants. To support the hematopoietic system, the introduction of vitamin B12 and folic acid is indicated.
If it was possible to cope with the disease, then the therapy ends. When autoimmune anemia reappears after some time, the patient is referred for surgery to remove the spleen. This will prevent the development of hemolytic crises in the future, since it is the spleen that is the “graveyard” for red blood cells in the human body. This procedure leads to complete recovery quite often, in about 74-85% of cases.
Immunosuppressive therapy is a last resort in the treatment of autoimmune anemia, which is resorted to only when splenectomy does not achieve the desired results.
Prevention and prognosis of the disease

In order to prevent the development of anemia, it is necessary to direct efforts to prevent human infection with dangerous viruses that can provoke the disease. If anemia has already developed, then it is necessary to minimize the impact on the body of those factors that can cause its exacerbation, for example, to avoid high or low temperatures.
It is impossible to prevent the development of idiopathic anemia, since its causes are unknown.
If the patient has suffered an episode of autoimmune anemia at least once, then for the next two years he must donate blood for a general analysis. This must be done at intervals of 3 months. Any symptoms that may indicate new anemia should be evaluated by a physician immediately.
In terms of prognosis, idiopathic anemia is more difficult to treat. Complete recovery after undergoing a hormonal course can be achieved in no more than 10% of patients. However, the removal of the spleen increases the number of recovered people up to 80%. Immunosuppressive therapy is difficult for patients to tolerate, such treatment negatively affects the immune system and causes multiple complications. The success of treatment largely depends on the factor that caused the development of anemia.









