Contents
Arthroplasty
Arthroplasty is a generic term encompassing the various surgical procedures consisting in replacing all or part of a diseased joint with a prosthesis. An arthroplasty can therefore be performed for different joints: the hip (the most common), the knee, the shoulder. Thanks to technological progress, prostheses today allow very good mobility, and have a satisfactory lifespan.
What is arthroplasty?
Arthroplasty refers to the surgical procedure consisting in replacing part or all of a painful and / or non-functional joint with a prosthesis. There are therefore different types of arthroplasty:
- Hip arthroplasty is the most common orthopedic surgery. It consists of replacing the hip with a total hip replacement (THA). This is composed of several elements: a cup fixed on the acetabulum (articular surface on the side of the pelvis) and a metal rod fixed in the femur comprising a head.
- Shoulder arthroplasty involves replacing the shoulder joint with a total shoulder prosthesis made up of two parts, a metal rod buried in the humerus and a glenoid part fixed in the scapula. Two types of shoulder prosthesis exist: the anatomical shoulder prosthesis, which reproduces the anatomy of the shoulder, and the reverse shoulder prosthesis. The second is preferred in the event of a major rupture of the rotator cuff associated with osteoarthritis of the shoulder. Unlike the anatomical prosthesis, the reverse prosthesis can be used when the cuff cannot be preserved because it is too damaged.
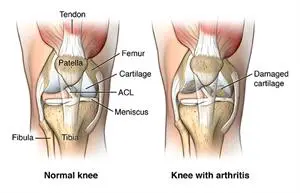
- Knee arthroplasty consists of replacing all or part of the knee joint with a prosthesis, either uni-compartmental (a half-prosthesis to replace the internal or external compartment of the knee) or total (replacing the two compartments of the knee joint: the femoro-tibial compartment and the femoro-patellar compartment).
These prostheses are available in different sizes and materials: metal, polyethylene, ceramic. Some are cemented, that is to say fixed with a specific glue, while others are impacted: they are covered with a mineral material that promotes the formation of bone cells, ultimately allowing fixation of implants. The surgeon chooses the most suitable prosthesis for his patient according to his age, his morphology, his degree of activity.
How does an arthroplasty work?
Before arthroplasty
An anesthetic assessment is carried out.
In order to ensure the absence of infection (contraindicating the intervention), a urinalysis and a dental check-up are prescribed before hospitalization. Measurements are also made to create trial prosthetic implants. A blood test and a cardiological assessment are carried out upon entry.
The intervention
Arthroplasty occurs under general or locoregional anesthesia.
Whether it concerns the hip, knee or shoulder, it follows the same operating pattern. On the skin area prepared and protected by sterile drapes, the surgeon makes an incision in order to access the damaged joint and remove it according to precise calculations. He then places trial prosthetic implants adapted to the patient’s morphology. If the result is satisfactory, he places the definitive implants. He tests them, then an X-ray is taken in the operating room to check their position.
A Redon drain is left in place to evacuate the various fluids (blood, lymph), then the incision is closed using staples.
In total, the procedure lasts from 1 hour to 1 hour 30 minutes.
When to perform an arthroplasty?
The most common indication for hip arthroplasty is coxarthrosis, or osteoarthritis of the hip. This can be either primary (it is then due to aging) or secondary (following hip dysplasia, aseptic osteonecrosis, post-traumatic disease, rheumatic disease, femoro-actetabular conflict, for example). The indication for arthroplasty is then made on a case-by-case basis, taking into account these different elements: the level of pain and the effectiveness of the analgesic treatment, the impact on function, assessed by self-administered scores (Harris , WOMAC, HOOS), the impact on quality of life (score SF-12) and 4), patient expectations. Hip replacement surgery can also be done for congenital hip dislocation
Shoulder arthroplasty has two main indications: osteoarthritis (omarthrosis) and massive and degenerative rupture of the generator cuff, two pathologies observed mainly in the elderly. The fitting of a total prosthesis is considered after failure of the first-line treatment: non-steroidal anti-inflammatory drugs, corticosteroid infiltration, physiotherapy.
Knee arthroplasty is also indicated in cases of primary or secondary osteoarthritis of the knee (gonarthrosis) (following an axial defect of the lower limb, a fracture, a pathology of the meniscus, a severe sprain), after failure of conservative treatment ( non-steroidal anti-inflammatory drugs, corticosteroid injections, viscosupplementation, osteotomy, arthroscopy cleaning).
Arthroplasty, whatever it is, then relieves pain and restores good joint mobility.
After arthroplasty
Operative suites
As soon as you return from the operating room, analgesic treatment is put in place to calm the pain. Anticoagulant therapy is also prescribed for the prevention of phlebitis (except for shoulder arthroplasty).
After hip arthroplasty, getting up is done on the first or second postoperative day, in the presence of a physiotherapist. Walking with full support is possible the day after or two days after the operation. The dressings are changed every two days, and the drain removed on the second day. The staples are removed a dozen days after the operation. During 3 months, certain actions are to be avoided in order to avoid dislocation of the hip. Rehabilitation in a center is not compulsory.
After shoulder arthroplasty, the shoulder is immobilized for 21 days in a splint, but a rehabilitation protocol is put in place from the first postoperative day. Rehabilitation in a specialized center is recommended.
After knee arthroplasty, getting up is done on the second postoperative day, in the presence of a physiotherapist. Walking is then possible with crutches. Rehabilitation in a specialized center is strongly recommended.
The risks
Although it is a common procedure, especially for the hip, arthroplasitis does carry different risks:
- phlebitis;
- hematoma ;
- an infection ;
- paralysis of a nerve affected during the procedure;
- residual pain;
- irritation of the tendons around the prosthesis;
- a keloid scar;
- a dislocation of the prosthesis (it dislocates);
- loosening of the prosthesis;
- a fracture during the operation. Rare, this complication mainly affects patients with severe osteoporosis.
Finally, it should be noted that when wearing a prosthesis, the patient must be vigilant against any infection. He must therefore consult in the presence of fever or infectious signs, and must in particular ensure his oral health.
Writing : Julie Martory, health journalist January 2019 |