Contents
What is knee arthritis?
Any inflammatory process has a great potential danger. The worst threat is sepsis. It is generally accepted that inflammation originates only in soft tissues. This is a very erroneous opinion, because. Increasingly, it affects the articulation of bones – the joints.
Arthritis of the knee – this is inflammation of the intra- and periarticular areas of one or both knees. Another name for the pathology is driving or gonarthrosis (from the Greek gony – “knee”).
The statistics of the incidence of arthritis of the knee joint is as follows: approximately half (from 35 to 52%) of people suffering from joint diseases suffer from knee arthritis. More than 30% – in children. And in 23% of all cases, the cause is osteoarthritis. Most patients with knee arthritis are women over 30 years of age. Although for secondary pathologies this is not always true. For example, gonorrheal arthritis is typical for men.
A high percentage of the likelihood of developing arthritis of the knee joint is caused by a high load on the knees. Each of them supports half the weight of the human body, and due to the very limited range of motion in the knees, this load only increases. The feet are more mobile and complex for this.
Diagnosis of pathology is carried out using radiography, or rather, arthrography. With pseudogout, polarizing microscopy of the synovial fluid obtained through a puncture is additionally required. On the microflora of punctate, the effect of various drugs on infectious pathogens is checked.
In rare cases, additional diagnostic studies are prescribed:

magnetic resonance imaging;
biopsy of the synovial membrane and cartilage;
thermography;
tomography;
arthropneumogram;
Wright reaction tests and Burne tests;
computed tomography – visualization of sequestered bone tissue. Sequester – dead area of bone tissue;
Magnetic resonance imaging;
ultrasound and radionuclide research.
Gradually, all the synovial tissues of the joint become inflamed. The cruciate ligaments undergo gross changes. The cartilage is destroyed. Spongy tissue is exposed, in which osteomyelitis or osteitis (“inflammation of the bone”) develops. Occurring changes are determined using radiographs.
Pathological abnormalities cover more and more organs over time:
bones;
tendons;
bursae;
ligaments;
cartilage;
muscles;
circulatory and lymphatic systems (lymphadenitis);
various internal organs.
The consequences of persecution can affect the functioning of many organs:
other joints – gonarthrosis, capsulitis, spondylitis (inflammation of the spine), bursitis, empyema, flexion contracture in a bent position, osteochondritis – an inflammatory process in bone and cartilage tissue;
eyes – keratitis, keratoconjunctivitis, uveitis;
lungs – alveolitis, pneumonitis, interstitial fibrosis;
heart – pericarditis, rheumatism, myocarditis;
blood vessels – systemic vasculitis, septic shock, provoking multiple organ failure syndrome, Raynaud’s syndrome, capillaritis;
gastrointestinal tract – enterocolitis;
kidneys – glomerulonephritis, amyloidosis.
The type of knee arthritis depends on what causes it. For example, purulent or septic inflammation is provoked by pathogens that enter the joint cavity from the primary foci of infection with blood or lymph. If both knees are affected, then they talk about Clutton’s joints.
There is no single classification of arthritis of the knee joint according to the causes of occurrence:

infectious;
reactive after suffering intestinal or urogenital infections;
juvenile rheumatoid, in which immunity destroys the cells of its own body, and rashes appear on the skin – rheumatic nodules at the knee and on the hand;
allergic (more often in the form of polyarthritis);
rheumatic (usually oligoarthritis);
psoriatic;
gouty;
streptococcal;
staphylococcal;
tuberculosis;
gonorrheal;
infectious-allergic;
immunoallergic;
post-traumatic;
exchange;
post-vaccination.
This classification is highly controversial. The disease can be acute or chronic. Some doctors also call a subacute form of the disease.
Depending on the localization of arthritis of the knee joint, there can be two types:
capsular or synovial affects the synovial membrane, usually proceeds in an acute form, often develops in children;
bone or dry affects the osteochondral ends of the joint.
The more the disease progresses, the larger the area it covers. Capsular knee arthritis (otherwise synovitis – synovitis genu) turns into bone and vice versa. Synovitis may be accompanied by the formation of rice bodies in the effusion. This intensifies the pain syndrome.
According to the nature of the effusion, synovial arthritis is divided into:
serous;
serous-purulent;
purulent.
According to the presence of pathogens in the articular cavity, gonarthritis is divided into two varieties:
septic;
aseptic, when the joint fluid is sterile.
Preventive measures for arthritis of the knee joint are standard – this is a healthy lifestyle, as well as compliance with sanitary rules and regulations, safety precautions during work. Particular care should be taken by those whose professional activities are associated with a long stay on their feet, as well as constant vibration.
The variety of clinical forms of gonarthritis is due to the extensive volume, magnitude of the load and the complexity of the device of the knee joint. Features of the course of the disease depend on the age, constitution, reactions of the body and human tissues to various influences.
Symptoms of knee arthritis

The following symptoms of the knee joint are distinguished:
stiffness, stiffness of the knee joints due to severe swelling and accumulation of effusion when going up / down stairs, squatting, driving a car and any movement that somehow involves the affected knee, i.e. the volume of passive and active mobility is greatly reduced;
pain in the anterior part of the knee, aggravated in positions with the greatest tension on the tendon (has a “mechanical” character);
heaviness in the leg;
massive swelling of soft tissues – dropsy;
accumulation of exudate in the joint cavity;
stretching of the capsule and ligaments;
hypertrophy of the synovial membrane with a fungous form;
redness and local increase in skin temperature within 5-7 cm;
spindle-shaped appearance of a sore leg;
proliferation of villi with infiltration, swelling and fibrous degeneration;
a symptom of balloting the patella (balloting cup) – when the leg is straightened, it seems to sink into the area of exudate accumulation, when bent, it “emerges” again;
Bonnet position of the joint (forced half-bent at a right angle due to muscle tension);
fever, hectic nature of body temperature;
chills;
sweating;
enlargement of regional lymph nodes;
general malaise, feeling of weakness;
drowsiness;
weakness, lethargy;
decreased appetite;
periarticular phlegmon in advanced cases (very likely to be fatal);
atrophy of adjacent muscles, for example, the quadriceps femoris muscle – Alexandrov’s symptom;
osteoporosis;
bone destruction of the condyles, patella and tibia, serration, the appearance of irregularly shaped focal patterns at the articular ends;
rheumatic carditis;
rheumatic chorea;
rheumatic dense, painless, inactive nodules in the subcutaneous tissue, fascia, aponeuroses and bursae;
abscesses – abscesses;
fistulas;
necrosis of soft tissues and cartilage;
fibrosis due to connective tissue degeneration of the bag;
compaction and thickening of periarticular tissues;
filling the joint with scar tissue;
erosion of articular surfaces;
ankylosis due to soldering of the articular surfaces of the connective tissue.
These pathological signs appear blurry or pronounced. They are usually divided into local and extra-articular. Not necessarily the manifestation of the entire symptom complex at once. It all depends on the type of disease and associated pathologies.
The patella or patella is a small bony “shield” that covers the top of the knee. It is linked to the thigh muscle and enhances its action. The patella is only part of the powerful stabilizing frame of the knee joint. It begins to bulge forward with excessive accumulation of effusion in the cavity of the diseased joint. In this case, the knees acquire a spherical shape. Condyles – semicircular protrusions of the thigh and lower leg.
Signs of arthritis of the knee joint are very similar to the symptoms of many bone diseases, as well as tumor-like neoplasms:
fibrous osteodystrophy;
giant cell osteoclastoma;
sarcoma;
pigmented villonodular synovitis;
synovioma.
The laboratory and instrumental signs of arthritis of the knee joint include:
an increase in ESR – erythrocyte sedimentation rate (or ROHE – erythrocyte sedimentation reaction), the number of leukocytes (mainly polymorphonuclear cells), eosinophils and platelets in the general blood test;
detection of C-reactive protein and seromucoids in a biochemical blood test;
detection of HLA-27 antigen, ?-2 and gamma globulins in blood serum;
a sharp increase in the number of plasma cells in the synovium;
cartilage degeneration, narrowing of the joint space, gummous process in the bones, erosion and nodes in the bone tissue, osteophytes (injure the synovial membrane), subchondral sclerosis (sclerotic rim around the tuberculous focus and sequesters inside it) on x-rays.
Stages of development of arthritis of the knee joint

There are 3 stages in the development of the disease:
The first stage, initial. prearthritic phase. Usually takes about 6 hours. The disease proceeds in a purely hyperemic form. The only symptom here is a painful syndrome, i.e. arthralgia.
The second stage, early arthritis. Arthritic phase – the height of the disease.
Signs of the second stage may appear cyclically:
cartilage begins to harden;
bone grows pathologically;
the synovial membrane becomes inflamed;
abscesses form;
the capsule of the joint thickens.
The third stage, advanced arthritis. The post-arthritis phase is the subsidence of the disease.
Signs of the third stage:
cartilage is becoming thinner and almost completely destroyed;
in their place, due to progressive zonal osteogenesis, bone outgrowths form;
cavities with a foreign substance appear in the bones;
the joint is destroyed;
tissue scarring occurs;
the leg takes a vicious position and shortens / lengthens;
the person becomes disabled.
At the last stage, arthritis becomes chronic. Relapses and exacerbations of the disease are possible. The pain syndrome can be aggravated by a sharp change in the weather. This property of the body is called meteosensitivity.
The knee joint is the largest in the human body and contains more synovial fluid than others. When pathogens enter it, the inflammatory process proceeds rapidly, which is why it is so important to stop the disease at the first stage. Otherwise, unpleasant consequences cannot be avoided.
Causes of knee arthritis
There are many causes of knee arthritis, including:
mechanical overload from friction in the anterior section and prolonged kneeling (“housewife’s knee”);
incorrect position of the bones, which means uneven distribution of the load on the joint;
rubella vaccination – post-vaccination arthritis;
prolonged hypothermia or frostbite of the legs;
trauma, for example, a bruise, fracture, crack, rupture of the articular meniscus or damage to the ligaments – post-traumatic gonarthrosis;
allergy (drug and serum disease) – allergic arthritis, for example, with urticaria or Quincke’s edema;
Reiter’s disease – a syndrome of arthritis, urethritis and conjunctivitis (mainly in young men);
brucellosis;
Behcet’s disease;
arthritis of other joints, for example, purulent or parasitic;
helminthic and protozoal invasions;
tuberculosis – tuberculous arthritis;
lobar inflammation of the lungs;
acute strepto-, pneumo- or staphylococcal infection – infectious or septic arthritis;
fungus;
gonorrhea;
chlamydia;
syphilis;
lyme disease;
lupus erythematosus;
psoriasis (very rare) – psoriatic arthritis;
hepatitis;
pyrophosphate arthropathy with calcification;
gout – a metabolic disease with the deposition of uric acid salts in the joints – metabolic or gouty arthritis;
ankylosing spondylitis – a hereditary disease of the musculoskeletal system;
capillarotoxicosis;
erythema nodosum;
collagenosis (very rare);
sarcoidosis;
leukemia;
hemophilia;
scurvy;
osteomyelitis;
angina;
scarlet fever;
otitis;
pharyngitis;
dermatomyositis.
It is sometimes quite difficult to identify the cause of arthritis, because. the inflammatory process progresses gradually and until the onset of pain, characteristic symptoms may be absent. The most severe form of arthritis of the knee joint is acute phlegmonous with purulent fusion of the surrounding soft tissues, a breakthrough of pus in the tissues of the thigh and lower leg.
Types of infectious agents:
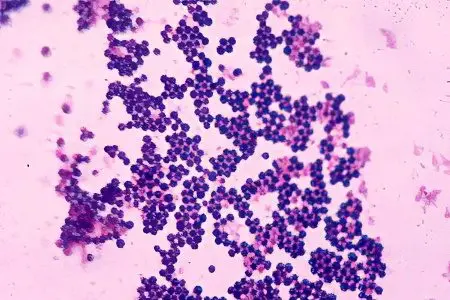
bacteria;
viruses;
parasites;
pathogenic fungi.
Bacteria:
staphylococcus;
gonococci;
streptococci;
hemophilus bacillus – Haemophilius influenzae;
gram-negative bacteria, such as Pseudomonas or salmonella – Salmonella.
Types of Staphylococcus:
Staphylococcus aureus;
epidermal staphylococcus – Staphylococcus epidermidis.
Types of Streptococcus:
β-hemolytic streptococcus of group A – Streptococcus pyogenes – is activated in gram-positive flora;
streptococci of other groups.
Viruses:
HIV, human immunodeficiency virus;
rubella;
epidemic parotitis;
hepatitis B;
parvoviruses.
Parasites are the causative agents of the following diseases:
opisthorchiasis;
strongyloidiasis – cochinchin diarrhea;
dracunculiasis – guinea worm disease;
hookworm – a rash of miners, earthen scabies or Egyptian chlorosis;
schistosomiasis;
echinococcosis liver;
filariasis, including wuchereriosis, brugiasis and onchocerciasis;
loiasis causing Calabar tumor.
So, the main varieties of bacterial infectious arthritis, depending on the etiology, are the causes of its occurrence:
gonococcal;
tuberculous primary bone or primary synovial form;
brucellosis;
borreliosis or lyme (for Lyme disease);
yersinia;
dysenteric;
salmonella.
Arthritis of the knee joint is divided into two types depending on the causes:
Primary (independent disease);
Secondary (associated with another pathology).
Risk factors or predisposing causes are:
prematurity;
excess weight;
heredity;
chronic foci of infection;
operative interventions;
gonorrhea – a sexually transmitted disease that affects the urinary tract;
furunculosis, accompanied by the appearance of boils;
peritonsillar abscess behind the tonsils;
angina – inflammation of the mucous membrane of the pharynx;
scarlet fever (mainly in childhood);
inflammation of the middle ear;
pneumonia – inflammation of the lungs;
infective endocarditis – inflammation of the endocardium – the inner lining of the heart;
immunodeficiency states;
recurrent septicemia;
joint prostheses;
diabetes mellitus – an endocrine disease due to insulin deficiency;
sickle cell anemia — anemia;
chronic tonsillitis – inflammation of the palatine tonsils;
caries – destruction of tooth tissues;
tumor;
hypogammaglobulinemia – protein deficiency;
alcohol addiction;
drug use;
congenital defects of the musculoskeletal system;
weak muscular frame of the knee joint;
extreme sports.
Symptoms of the disease are very different depending on the causes of its occurrence. So, if it is prolonged mechanical friction, then arthritis usually occurs without fever. With severe arthritis of the knee joints, you can completely lose the ability to move around.
How to treat knee arthritis?

The complex of therapeutic measures includes:
removal of inflammation (NSAIDs – non-steroidal anti-inflammatory drugs);
anesthesia;
restoration of metabolic processes (taking chondroprotectors, vitamins and immunostimulants);
strengthening immunity;
normalization of nutrition of articular tissues;
getting rid of excess weight (auriculotherapy, diet, herbal medicine to improve metabolic processes and break down fat deposits to reduce the load on the knees);
restoration of normal motor activity, support ability of the lower extremities, resumption of the full range of motion;
preventive measures to prevent recurrence of the disease.
Not only medications can help reduce pain, but also supportive aids such as a cane or crutches. Orthopedic devices are also used, such as knee pads, splints and special shoes. The leg is also immobilized with a simple plaster, coxite bandage or a splint made from a plaster cast.
With a secondary disease, priority measures are aimed at eliminating the underlying disease. Treatment is complex.
Non-steroidal anti-inflammatory drugs:
Ibuprofen. Pros: safe, less side effects than other drugs; rarely causes agranulocytosis in the blood. Cons: the antipyretic and analgesic effect is less than that of Paracetamol; can provoke the appearance of edema, hypertension, aspirin asthma, stomach ulcers, damage to the liver and kidneys;
Naproxen. Pros: has few side effects; highly effective. Cons: greater risk of cardiovascular complications than ibuprofen;
Aspirin or Acetylsalicylic acid. Pros: good antipyretic ability; prevents thrombosis (anti-aggregation or “anti-gluing” platelets in inflammation drug). Cons: does not help with pain; can cause Reye’s syndrome, which affects the liver and brain;
Paracetamol. Pros: the only remedy, without the risk of swelling and hypertension; rarely destroys the gastric mucosa; relieves pain and fever better than others. Cons: with age, the effect of the drug weakens; quickly wears out the liver, tk. is activated in it;
Admiral, Ortofen or Diclofenac. Pros: Quickly relieves arthritis pain. Cons: significantly increases the likelihood of a stroke; strongly plants the kidneys; negatively affects the gastrointestinal tract;
Olfen – a drug based on diclofenac sodium;
Nimesulide. Pros: effective tool; well tolerated; the total number of complications from the stomach and intestines is lower than that of analogues. Cons: no accurate data on the cardiovascular safety of the drug;
Revmoxicam or Meloxicam. Pros: gives a significant improvement; easily tolerated. Cons: insufficiently studied cardiovascular safety; high relative risk of bleeding.
In the treatment of infectious gonitis, Lincomycin is often used – an antibiotic, an antimicrobial drug. Pros: copes well with pathogens, mycoplasma, bacteroids. Cons: Can cause nausea, vomiting, diarrhea, stomatitis and other complications.
Ointments for arthritis of the knee joint:
Finalized;
Apizartron;
Histalgon.
Corticosteroids – steroid hormones – are injected directly into the joint cavity:
Hydrocortisone in the form of a suspension;
Kenalog;
Trasilol or Aprotinin;
Diprospan.
Immunostimulants for gonarthritis:
Levamisole or Decaris. Pros: increases immunity, scars ulcers. Cons: provokes a headache, disrupts sleep;
Taktivin in solution;
Methyluracil. Pros: accelerates wound healing; usually well tolerated. Cons: allergic skin reactions, dizziness are possible.
Chondroprotectors are taken in long courses even after the end of the main treatment. They significantly accelerate cell regeneration. If arthritis is provoked by an infectious agent, then antibiotic therapy (etiotropic) is performed. Additionally, immunostimulants and antitoxic agents are administered.
Forms of medications prescribed for arthritis of the knee joint:
tablets (for example, Diclofenac);
solutions for intramuscular and intraarticular injections (for example, corticosteroids);
gels (for example, Diklak);
cream;
ointments (for example, Bishofit, Nikoflex, Menovazin);
solutions for lotions (for example, Dimexide).
These drugs have many side effects, overload the gastrointestinal tract, so at the same time as they are taken, it is necessary to follow a diet and prescribe drugs that support the digestive process.
If an abscess occurs, it must be punctured. Otherwise, a fistula is formed. In the absence of sequesters, fistulas are amenable to iodoform sealing according to Mosetig-Moorhof. Accelerates the healing process of quartzing.
To correct the resulting deformities of the knees, i.e. O- and X-shaped legs, orthopedic correction methods are used. In case of contracture, gonitas require constant limb extension or light one-stage redressing with plaster fixation. Advanced cases can be straightened with the Ermolaev apparatus or corrected by supracondylar osteotomy.
Correction of bone deformities is possible only by surgery. Types of surgical interventions when driving:
replantation of the synovial membrane of the joint;
cartilage transplantation;
arthroscopy – removal of processes from the bone and other manipulations through a micro incision;
endoprosthetics – replacement of joint components with implants;
arthrodesis – complete immobilization of the joint;
arthrolysis or Wolff’s operation – excision of fibrous adhesions;
synovectomy – removal of the affected synovial membrane;
washing the joint;
alignment of the menisci (these are semilunar cartilaginous formations, additional shock absorbers of the legs);
arthroplasty – partial or complete prosthetic replacement of a joint;
osteotomy – removal of part of the bone in order to reduce pressure on the joint;
intra-articular necrectomy;
plastic resection – removal of a joint or part of it – a knee of a closed or open type with fascial interposition;
wide bilateral parapatellar arthrotomy.
In severe cases, a resection, wedge osteotomy or arthroplasty is done a second time. Resections and neararthrosis should not be done until the age of 17. If the growth zones of the bones of the lower extremities are damaged, the child will forever remain lame.
Some therapeutic techniques are used only under the condition of getting rid of pain and inflammation. Among them are the methods of Tibetan medicine:

physiotherapy;
massage and self-massage to relax the muscular frame of the knee and increase blood circulation;
pharmacopuncture – the introduction of drugs in minimal doses into biologically active points of the back;
acupuncture or needle therapy;
auriculotherapy – the introduction of needles into the biologically active points of the ears;
medical and physical culture complex;
health resort recovery.
The following physiotherapy procedures are prescribed:
phonophoresis with hydrocortisone;
paraffin applications;
magnet;
quartzing;
laser;
UHF;
radon or hydrogen sulfide baths.
It is forbidden!:
self-medicate;
endure pain or constantly relieve it with analgesics and do not seek help from specialists;
in the secondary drive to treat only him, ignoring the disease-root cause.
Large articulations of the bones of the lower extremities are at risk of an inflammatory process, often only because of the negligence of the person himself. Working without observing the simplest sanitary rules and norms, without sparing yourself, can only have a negative effect on health. Without timely suppression of chronic infectious foci in the body, a person dooms himself to long-term treatment and the occurrence of various complications.
Just 1 simple exercise heals the knees – Dr. Evdokimenko:









