Contents
- Why take a stool test for dysbacteriosis?
- Preparation for the study and collection of material
- Analysis of feces for dysbacteriosis in infants
- Table of norms for bacteriological analysis of feces
- Deciphering the results of the study
- Bifidobacteria
- lactobacteria
- Peptostreptococci
- Escherichia typical
- Escherichia lactosonegative
- Fusobacteria
- Bacteroid
- eubacteria
- Enterococci
- Staphylococcus saprophytic and epidermal
- Waylonelles
- Clostridia
- candida
- Other opportunistic bacteria
- salmonella
- Shigella
- Yersinia
- Pseudomonas aeruginosa
- Hemolytic Escherichia
- Staphylococcus aureus

In the intestines of an adult, on average, from 2,5 to 3,5 kg of various bacteria live. The totality of these microorganisms is called microflora, and our health and well-being directly depend on the ratio of the number of its individual representatives. An imbalance in the intestinal microflora or simply dysbacteriosis is a very common problem in the modern world, but it is a mistake to consider it an independent disease. From the point of view of the medical community, dysbacteriosis is only a condition (most often temporary), against which a person can develop diseases. To prevent this from happening, at the first characteristic signs of trouble in the intestines, it is recommended to take a stool test for dysbacteriosis, the decoding of the results of which will allow the doctor to decide on further diagnostic and therapeutic tactics.
Success largely depends on how carefully the patient prepared for the stool test and whether he collected the material correctly. When it comes to diagnosing intestinal dysbiosis in infants and young children, there is a need to discuss some subtleties. Today we will tell you what signs and symptoms are indications for such a study, what the analysis of feces for dysbacteriosis shows (decoding of the results and norms in the table), what methods determine the imbalance of the intestinal microflora, for what reason they occur and what consequences they can lead to .
Please note that the information provided is for informational purposes only and does not replace the need for qualified medical assistance. Dysbacteriosis is a serious pathological condition that has a detrimental effect on digestion, metabolism, immune status and many other aspects of human health, and therefore requires a visit to a doctor!
Why take a stool test for dysbacteriosis?

The trillions of bacteria living in our body are in symbiotic interaction with us, that is, they receive their benefit from the host, while simultaneously benefiting him. But this statement is true in relation to all microorganisms to varying degrees: some of them are more welcome guests for humans, some are less, and some are completely “persona non grata”. An analysis of feces for dysbacteriosis is precisely carried out in order to establish the numerical ratio between the colonies of bacteria that inhabit the intestines.
Indications for the purpose of the study:
diarrhea or constipation;
Nausea and vomiting;
Flatulence;
Heaviness, discomfort, bloating, abdominal pain;
Suspicion of an intestinal infection;
Sudden weight loss for no apparent reason;
Intolerance to certain foods;
Allergic reactions, skin rashes;
Visible pathological impurities in the feces (mucus, blood, pus).
It is highly desirable to take a stool test for dysbacteriosis after undergoing long-term therapy with antibacterial or hormonal agents – deciphering the results of the study will determine how much the treatment affected the composition of the intestinal microflora, whether its correction is required.
Three methods are used for this:
Coproscopy – a kind of “general analysis of feces”, the very first step in the diagnosis of intestinal disorders. The result of the study is a coprogram – a form with indicators, including the color, shape, consistency and smell of feces, information about the presence or absence of latent blood, pus, mucus, parasites and their eggs, undigested food residues, atypical cells and tissue fragments. If the result is alarming, the doctor prescribes additional diagnostic procedures;
Bacteriological analysis of feces – in other words, sowing in a nutrient medium. After 4-5 days, the bacteria will multiply, and the laboratory assistant will be able to draw a conclusion about the number of the main representatives of the intestinal microflora in 1 gram of the material (CFU/g). It is this study that we are talking about today – it is simple and affordable, performed in any hospital and still serves as the leading way to determine dysbacteriosis in children and adults. However, such an analysis requires very strict adherence to the rules for the preparation and collection of material, and also takes too much time, so an alternative method was invented;
Biochemical analysis of feces is a modern diagnostic procedure based on gas-liquid chromatography of fatty acids by spectrum. Deciphering the results of the study becomes possible after a few hours, it reflects, among other things, the balance of the parietal microflora of the intestine. Fecal biochemistry is a more sensitive and accurate technique, even yesterday’s sample is suitable for it, since the fatty acids secreted by bacteria during their life activity remain unchanged for a long time. Biochemical analysis of feces for dysbacteriosis even allows you to establish a specific section of the intestine in which the failure occurred. The only drawback of the method is that it is not available in every laboratory.
The norms of biochemical analysis of feces are presented in the table:
Index | Absolute value (mg/g) | Relative value (unit) |
Acetic acid (C2) | 5,35-6,41 | 0,612-0,656 |
Propionic acid (C3) | 1,63-1,95 | 0,180-0,198 |
Butyric acid (C4) | 1,60-1,90 | 0,167-0,185 |
IsoCn/Cn | 0,29-0,57 | 0,30-0,60 |
Total acid content | 8,01-13,01 | 9,00-12,01 |
Anaerobic index | from -0,686 to -0,466 | from -0,576 to -0,578 |
Preparation for the study and collection of material

It is very important not only to correctly collect feces for analysis for dysbacteriosis, but also to deliver the sample on time, as well as to observe all the details of preparation.
Let’s start in order:
If you have been treated with antibiotics, keep in mind that it makes sense to take a stool test to determine imbalances in the intestinal microflora no earlier than two weeks after the end of therapy;
Three days before the examination, it is necessary to abandon the use of laxatives, antidiarrheal and anthelmintic drugs, NSAIDs, pro- and prebiotics, castor and vaseline oils, barium and bismuth preparations;
It is necessary to purchase in advance at the pharmacy or get in the laboratory a sterile plastic container with a spoon and a tight-fitting lid, specially designed for collecting and transporting feces for analysis;
Defecation should take place naturally, without the use of enemas or any other aids;
Do not collect a sample for analysis from a toilet bowl. For these purposes, you need to prepare any convenient container, which should be thoroughly washed, poured over with boiling water, dried, and defecate into it;
Before starting the process, you must urinate, then wash and dry yourself. In no case should the collected sample contain urine or secretions from the genital tract. If a woman is menstruating, a tampon should be used;
When defecation has taken place, it is necessary to open the prepared container, take a spoon and collect a little bit of material from different parts of the stool: from the middle, from the surface. If you see a suspicious area containing mucus or blood that differs in consistency or color from the surrounding feces, be sure to place it in a container! In total, 6-8 spoons of feces will be needed for analysis;
Close the container tightly and deliver the sample to the laboratory no later than 2 hours after collection.
If you are undergoing a biochemical study, the urgency is not so significant – you can even freeze the sample and bring it to the laboratory the next day. This is especially convenient for parents of infants and small children, because it is not known whether it will be possible to collect feces from a child for analysis early in the morning – perhaps he simply does not want to go to the toilet.
Analysis of feces for dysbacteriosis in infants

The norms of bacteriological examination of feces in newborns, infants and older children are somewhat different from the same indicators in adults, and the younger the child, the more pronounced these differences. They are associated with the gradual colonization of the child’s body by bacteria. And this process, in turn, takes place in different ways in babies who are naturally or artificially fed. We will talk about this in more detail when deciphering the results of the analysis of feces for dysbacteriosis in the table.
The composition of the intestinal microflora of infants may undergo undesirable changes due to infection with nosocomial infections: Staphylococcus aureus, Pseudomonas aeruginosa, yeast-like fungi, and so on. At best, this will lead to temporary and minor health problems, and at worst, to a serious illness. Therefore, parents need to carefully monitor the behavior and well-being of the baby, the condition of his skin and mucous membranes, the frequency and appearance of bowel movements, especially if you have recently had a chance to undergo treatment in a hospital.
It is necessary to take a stool test for dysbacteriosis in an infant if the following symptoms are present:
Frequent and severe eructation after feeding, more like vomiting;
Bloating and colic in the abdomen, flatulence;
poor appetite;
Difficulties with the introduction of complementary foods;
Signs of intolerance to individual products;
Rashes, spots on the skin and / or mucous membranes;
Recent antibiotic or hormonal therapy;
Any problems with the stool – frequency disturbances, abnormal appearance or smell of feces, the presence of pathological impurities (blood, mucus, pus).
In order for the decoding of the results of the study to give objective results, it is necessary to properly prepare for the analysis:
Refuse to introduce new complementary foods at least 3-4 days before the visit to the laboratory;
On the eve, do not give your baby vegetables or fruits that can change the color of bowel movements (carrot puree, red and black berries, beetroot juice, and so on);
Stop taking any medications a few days before the test, including laxatives and vitamins. It is desirable to finish antibiotic therapy 2 weeks before the study. It is better to inform the doctor about all the medicines taken by the child and consult on the timing of the analysis of feces for dysbacteriosis;
Get a sterile plastic container with a spoon. It is acceptable to take a sample of baby stool from the surface of the diaper, but only if the filler is not gel. It is better to use a clean cotton diaper, before ironing it with a hot iron. To conduct the study, it is enough to collect 2 spoons of material.
Table of norms for bacteriological analysis of feces
flora type | Index | Babies | Children over 1 year old | Adults |
Useful flora | Bifidobacteria | 1010 – 1011 | 109 – 1010 | 108 – 1010 |
lactobacteria | 106 – 107 | 107 – 108 | 106 – 108 | |
Conditionally pathogenic flora | Peptostreptococci | 103 – 105 | 105 – 106 | 105 – 106 |
Escherichia typical | 106 – 107 | 107 – 108 | 106 – 108 | |
Escherichia lactosonegative | ≤105 | ≤105 | ≤105 | |
Fusobacteria | ≤106 | 108 – 109 | 108 – 109 | |
Bacteroid | 107 – 108 | 109 – 1010 | 109 – 1010 | |
eubacteria | 106 – 107 | 109 – 1010 | 109 – 1010 | |
Enterococci | 105 – 107 | 105 – 108 | 105 – 108 | |
Staphylococcus saprophytic and epidermal | ≤104 | ≤104 | ≤104 | |
Waylonelles | ≤105 | 105 – 106 | 105 – 106 | |
Clostridia | ≤103 | ≤105 | ≤105 | |
candida | ≤103 | ≤104 | ≤104 | |
Other opportunistic bacteria | ≤104 | ≤104 | ≤104 | |
Pathogenic flora | salmonella | negative (none) | negative (none) | negative (none) |
Shigella | negative (none) | negative (none) | negative (none) | |
Yersinia | negative (none) | negative (none) | negative (none) | |
Pseudomonas aeruginosa | negative (none) | negative (none) | negative (none) | |
Hemolytic Escherichia | negative (none) | negative (none) | negative (none) | |
Staphylococcus aureus | negative (none) | negative (none) | negative (none) |
Deciphering the results of the study

All intestinal microflora can be divided into three groups:
Beneficial bacteria – they play an extremely positive role in the life of the human body, so it is very important that they be enough. We are talking about bifidobacteria and lactobacilli;
Opportunistic bacteria – some of them, being in balance with other participants in the microflora, even bring certain benefits. But as soon as their colonies multiply too much, and the colonies of antagonists thin out, these bacteria turn from conditional enemies into real enemies. Especially often this happens against the background of a decrease in immune protection. We are talking, for example, about candida, enterococci or clostridia;
Pathogenic bacteria – they should not be in the body of a healthy person. There is no benefit from them, only problems. If the immune system fails to cope with the attack of such microorganisms, this will lead to the development of a serious disease. We are talking about Staphylococcus aureus, salmonella, shigella and other “unwanted guests” of the intestine.
Now consider the main representatives of the intestinal microflora in more detail. In the form with the results of the analysis of feces for dysbacteriosis, some of the following bacteria may be absent – laboratories have different rules, especially private ones. Therefore, it is better to entrust the decoding of the indicators to a qualified doctor, and here we just give the established norms and indicate the reasons for possible deviations.
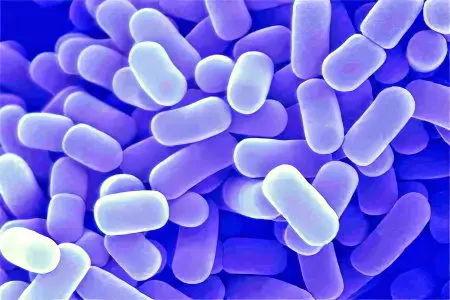
Bifidobacteria

The name of this microorganism comes from the Latin words “bacterium” and “bifidus”, that is, “divided in two.” Indeed, bifidobacteria has the form of a curved stick 2-5 microns long, forked at the ends. It belongs to the class of gram-positive anaerobes. The intestinal microflora of a healthy person is approximately 95% composed of bifidobacteria. The norms for babies up to a year are 10 to the tenth or eleventh degree CFU / g, and for older children and adults – 10 to the ninth or tenth degree CFU / g.
Deficiency of these beneficial bacteria is the main reason for going to the doctor with complaints of intestinal problems and referral for fecal analysis for dysbacteriosis – deciphering the results almost always indicates a decrease in their number. Without a sufficient amount of bifidobacteria, the absorption of vitamins and microelements is disrupted, carbohydrate metabolism suffers, local immunity decreases, and the toxic load of the liver and kidneys increases. Correcting the intestinal microflora and replenishing the deficiency of bifidobacteria is quite simple – there are many specialized preparations for this.
Bifidobacteria in feces are reduced – causes:
Long-term therapy with antibiotics, hormones, NSAIDs, laxatives, antihelminthics;
Irrational nutrition – an excess of carbohydrates or fats in the diet, starvation, rigid mono-diets;
Artificial feeding of infants, too early introduction of complementary foods;
Congenital fermentopathy – intolerance to lactose, fructose, gluten and other food components;
Immunodeficiency states, allergies;
Intestinal infections – dysentery, salmonellosis, yersiniosis;
Parasitic invasions – ascariasis, enterobiasis, giardiasis;
Chronic diseases of the gastrointestinal tract – enterocolitis, cholecystitis, gastritis, pancreatitis, stomach ulcer;
emotional stress;
Abrupt climate change.
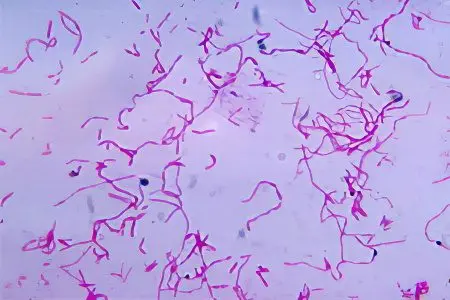
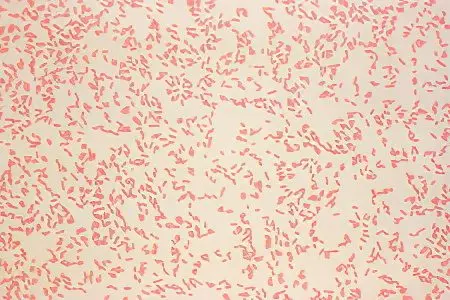
lactobacteria
The name of these beneficial members of the intestinal microflora comes from the Latin word “lac”, which means “milk”. There are many species of them that inhabit, including other internal organs, for example, female genital organs. Lactobacilli are gram-positive facultative anaerobic microorganisms, look like thin sticks and make up about 3% of the total mass of all bacteria living in the intestine. According to the decoding of the analysis of feces for dysbacteriosis, the norm of their content in infants is 10 to the sixth or seventh degree CFU / g, and in adult patients – 10 to the seventh or eighth degree CFU / g.
Lactobacilli produce organic acids, thereby maintaining the correct pH balance in the intestines. In addition, they are involved in membrane digestion, namely, they break down milk sugar, preventing the occurrence of lactase deficiency. Normal assimilation of milk is in principle impossible without a sufficient amount of lactobacilli. A person also needs them as stimulants of local immunity, because, being foreign elements, they spur the activity of immunocompetent cells that inhabit the parietal zone of the intestine. Lactobacilli are also involved in the metabolism of bile acids, contribute to normal peristalsis, prevent feces from becoming too hard, and therefore indirectly prevent the development of constipation.
Lactobacilli in feces are reduced – causes:
Long-term antibiotic therapy without the support of pre- and probiotics, uncontrolled use of NSAIDs (aspirin, analgin, ibuprofen), the use of laxatives or anthelmintic drugs;
Unbalanced diet, starvation, mono-diets;
Artificial feeding or too early introduction of complementary foods in infants;
Acute intestinal infections;
Chronic gastrointestinal diseases;
Strong stress.
Peptostreptococci

These bacteria belong to the opportunistic flora, they are small round-shaped cells that stray into short chains and are able to move with the help of movement organelles – cilia. Peptostreptococci are gram-positive non-spore-forming anaerobes, they live in the oral cavity, vagina, intestines and on the skin, while accounting for up to 18% of all gram-positive anaerobic cocci living in the human body. When deciphering the results of fecal analysis for dysbacteriosis, the norm for peptostreptococci in children under one year old is a maximum of 10 to the fifth degree CFU / g, and in adults – a maximum of 10 to the sixth degree CFU / g.
Peptostreptococci play a modest role in the metabolism of proteins and carbohydrates, as well as the production of hydrogen, which is necessary to maintain a healthy acid-base balance in the intestine. However, their number must be strictly controlled by the immune system and other members of the microflora. Excessively multiplied colonies of peptostreptococci can cause mixed abdominal infections together with other opportunistic and pathogenic bacterial strains. For example, peptostreptococci appear in 20% of cases of peritonitis. They are also sown in gynecological inflammatory diseases, as well as in purulent abscesses in the oral cavity.
Peptostreptococci in feces are increased – causes:
Acute intestinal infection;
Chronic diseases of the gastrointestinal tract;
Too much sugar in the diet.
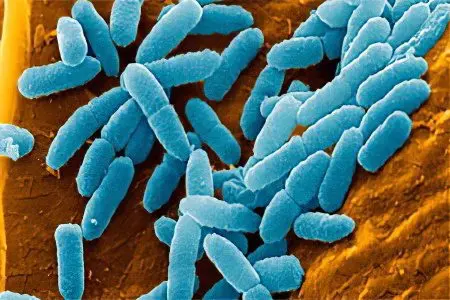
Escherichia typical
Escherichia coli (Escherichia coli, Escherichia typical) is a gram-negative facultative anaerobic non-spore-forming bacterium, most strains of which are conditionally pathogenic and act as a natural participant in the microflora of internal organs. Already within the first forty hours after birth, the intestines of the child are populated by Escherichia. When deciphering the results of a fecal analysis for dysbacteriosis, the E. coli content in infants is 10 to the sixth or seventh degree CFU / g, and in older babies and adults – 10 to the seventh or eighth degree CFU / g. In comparison with other microorganisms, E. coli forms up to 1% of the total mass of bacteria living in the intestine.
A typical Escherichia benefits a person: it is involved in the synthesis of vitamins B and K, in the metabolism of cholesterol, bilirubin and choline, in the process of absorption of iron and calcium. E. coli produces a number of essential acids (acetic, lactic, succinic, formic), colicin substances that are harmful to pathogenic bacteria, and also takes excess oxygen from the intestine, which is harmful to lactobacilli and bifidobacteria. That is why, despite the opportunistic status of E. coli, its deficiency is highly undesirable.
Escherichia in the feces are lowered – the reasons:
Long-term therapy with antibacterial drugs;
Acute intestinal infection;
parasitic invasion;
Unbalanced diet;
Artificial feeding of babies.
Escherichia lactosonegative

The presence of this strain in the interpretation of the results of the analysis of feces for dysbacteriosis is quite acceptable. The norm for the content of lactose-negative Escherichia coli in the intestines of children and adults is no more than 10 to the fifth degree CFU / g.
Exceeding this indicator is an alarming sign, especially in combination with a deficiency of full-fledged Escherichia. The lactose-negative strain does not perform the functions that are assigned to E. coli, but simply takes up space to no avail. In conditions of reduced immunity, E. coli – “parasite” will act on the side of harmful bacteria and aggravate the course of the inflammatory process, if one begins. In young children, an increased content of lactose-negative Escherichia in the feces indirectly indicates helminthic invasion, so a similar result of the analysis requires additional examination.
Fusobacteria
They belong to gram-negative anaerobes, are polymorphic, and do not have organelles of movement, do not form spores and capsules. In appearance, fusobacteria are thin sticks 2-3 microns long with pointed ends. These are natural participants in the microflora of the oral cavity, upper respiratory tract, gastrointestinal tract and genital organs. According to the norms of analysis of feces for dysbacteriosis, in the intestines of infants, the content of fusobacteria is allowed up to 10 to the sixth degree CFU / g, adult patients – up to 10 to the eighth degree CFU / g.
Fusobacteria are conditionally pathogenic, while they do not perform any useful function in the human body, unless they enter into competitive interaction with other, more potentially dangerous microorganisms. Some types of fusobacteria in conditions of immunodeficiency are capable of provoking purulent-septic inflammations. In debilitated children and the elderly with severe angina, a formidable complication can develop – fusospirochetosis. This is a necrotic process that affects the mucous membranes of the mouth and throat.
Bacteroid
These are opportunistic gram-negative rod-shaped anaerobes. They are the second largest members of the natural intestinal microflora after bifidobacteria. Deciphering the results of fecal analysis for dysbacteriosis implies the following norms for bacteroids: in children under one year old – 10 to the seventh or eighth degree CFU / g, in adult patients – 10 to the ninth or 10 to the tenth degree CFU / g. It is noteworthy that in babies up to 6-8 months of age, these bacteria are not sown, especially if the child is breastfed and does not receive early complementary foods.
Bacteroids in normal concentration are useful – they take part in the metabolism of fats. But if they multiply excessively, they will begin to compete with E. coli for oxygen, and this threatens with digestive disorders, vitamin and microelement deficiencies, decreased local immunity and other problems (we talked about the beneficial role of typical Escherichia above). The growth of the population of bacteroids is restrained by their direct antagonists – lactobacilli and bifidobacteria. Therefore, if the results of the analysis of feces for dysbacteriosis indicate an excess of the concentration of bacteroids in the intestine, it is recommended to drink a course of appropriate drugs to restore healthy microflora.
Bacteroids in feces are increased – causes:
Excessive consumption of fats;
Deficiency of bifido- and lactobacilli.
Bacteroids in feces are reduced – reasons:
Long-term therapy with antibacterial agents;
Acute intestinal infection;
parasitic invasion.
eubacteria
Gram-positive anaerobes, shaped like thick short columns or flattened spheres, have rigid cell walls, do not form spores. Eubacteria are representatives of the natural intestinal microflora, however, they are opportunistic, since some of their strains can provoke inflammatory processes in the oral cavity, respiratory system, genitals, joints, heart, brain, and can also cause postoperative complications. The norms for the content of eubacteria in the intestine when deciphering the results of fecal analysis for dysbacteriosis are as follows: for infants – 10 to the sixth or seventh degree CFU / g, for older children, adults and the elderly – 10 to the ninth or tenth degree CFU / g.
From these figures, it becomes obvious that eubacteria are a fairly numerous representative of the intestinal microflora. It is noteworthy that in breastfed babies under one year old, these bacteria are rarely sown, while in artificial children they are almost always present. Eubacteria in the right concentration are useful for the body – they are involved in the metabolism of cholesterol and hormonal metabolism, synthesize important organic acids, ferment carbohydrates, produce vitamins, and break down cellulose. However, their excessive amount, especially in conditions of reduced immune protection, can be hazardous to health.
Enterococci
Gram-positive facultative anaerobic cocci habitually paired or in chains that do not form spores. Enterococci belong to the conditionally pathogenic flora, are present in the intestines of people of any age and make up to 25% of all coccal forms living there. Normal indicators of the content of enterococci in deciphering the analysis of feces for dysbacteriosis: in infants – from 10 to the fifth degree to 10 to the seventh degree CFU / g, in older children and adult patients – from 10 to the fifth degree to 10 to the eighth degree CFU / g.
Enterococci perform some useful functions: they are involved in carbohydrate metabolism, vitamin synthesis, and maintaining local immunity. However, the population of enterococci should not exceed the population of Escherichia coli, otherwise the latter will begin to die in a competitive confrontation. The opinion of doctors regarding the harmlessness of enterococci has recently lost its relevance. Mutated strains have emerged that are resistant to the most powerful antibiotics: beta-lactam penicillins, cephalosporins, aminoglycosides, and even vancomycin. Cases of nosocomial infections, postoperative complications and inflammatory diseases caused by enterococci, including meningitis and endocarditis, are known.
Enterococci in feces are increased – causes:
Autoimmune pathologies;
Immunodeficiency states;
Allergy;
parasitic infestations;
Irrational nutrition;
Long-term antibiotic therapy;
Lack of Escherichia coli.
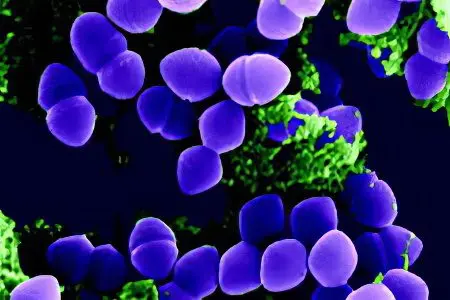
Staphylococcus saprophytic and epidermal
Gram-positive facultative anaerobic cocci up to 1,2 µm in diameter, non-spore-forming, immobile, grouped like grapes. Saprophytic staphylococcus lives mainly in the genitourinary tract, and epidermal, as the name implies, on the surface of the skin and mucous membranes. Both of these species belong to opportunistic microflora and can normally be present in deciphering the results of fecal analysis for dysbacteriosis: up to 10 to the fourth degree CFU / g in children and adults.
As long as these staphylococci are controlled by the immune system, they cannot cause significant harm to human health. But they are of no use either. Colonies of saprophytic staphylococcus that have multiplied in the intestines can cause acute cystitis or urethritis with improper wiping after the toilet, and epidermal – for example, conjunctivitis as a result of rubbing the eyes with dirty hands. Exceeding the content of these types of staphylococcus in the feces is definitely an unfavorable sign, and if it is significant, then the patient may need antibiotic therapy.
Waylonelles
Gram-negative anaerobic cocci, very small, immobile and non-spore-forming, habitually grouped in irregular spots. Veillonella are opportunistic microorganisms and peacefully coexist with humans, however, some of their strains can provoke purulent-septic inflammatory processes. When deciphering the results of fecal analysis for dysbacteriosis, the following norms are used: for babies up to a year – less than or equal to 10 to the fifth degree CFU / g, for older children and adults – 10 to the fifth or sixth degree CFU / g. It is noteworthy that under the condition of natural feeding, veillonella is sown in less than half of the babies.
These bacteria have a useful function – they break down lactic acid. In addition, there are scientific studies that indicate an indirect relationship between veillonell deficiency and the risk of developing asthma in children. But there are species of these bacteria that have pronounced periodontogenic properties – microbes accumulate in dental plaques, cause inflammation of the gums and loss of teeth. And, for example, Veillonella parvula provokes colitis in humans. In addition, even beneficial strains of veillonella in conditions of overabundance in the intestines lead to increased gas formation, dyspepsia and diarrhea.
Clostridia
Gram-positive obligate anaerobic rod-shaped bacteria capable of reproducing by endospores. The name “clostridia” comes from the Greek word for “spindle”, and this is not accidental: located in the center of the dispute, as a rule, it has a larger diameter than the cell itself, which is why it swells and becomes like a spindle. The genus Clostridia is very numerous – among them there are both representatives of conditionally pathogenic flora and pathogens of dangerous diseases (tetanus, botulism, gas gangrene). The norm of the content of clostridia in the feces when deciphering the analysis for dysbacteriosis is as follows: in infants – no more than 10 to the third degree CFU / g, in adults – no more than 10 to the fourth degree CFU / g.
Clostridia perform a useful function – they are involved in the metabolism of proteins. Metabolic products are substances called indole and skatole. In fact, these are poisons, but in small quantities they stimulate peristalsis, promoting fecal masses and preventing the development of constipation. If the concentration of clostridia in the intestine is too high, it will lead to putrefactive dyspepsia, the striking symptoms of which are watery diarrhea with a rotten smell, nausea, bloating, flatulence, colic, and sometimes fever. Against the background of weakened immunity and in association with other pathogenic bacteria, clostridia can cause necrotizing enterocolitis, cystitis, urethritis, vaginitis, prostatitis, and many other inflammatory diseases.
candida
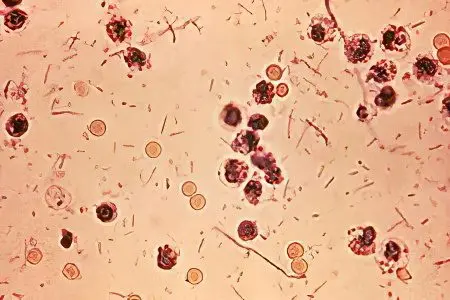
Yeast-like fungi-deuteromycetes, unicellular microorganisms of a round or oval shape, forming pseudomycelium, that is, long thin threads. The most common species are Candida albicans and Candida tropicalis. They inhabit the human body during the first year of life, live on the mucous membranes of the oral cavity and genital organs, as well as in the intestines. Candida is a bright representative of conditionally pathogenic flora. When deciphering the results of fecal analysis for dysbacteriosis, it is customary to adhere to the following standards: no more than 10 to the fourth degree CFU / g for patients of any age.
Candida are involved in the regulation of pH levels, so if their number is within acceptable limits, they benefit a person. But if yeast-like fungi multiply too much, this will lead to the development of local or even systemic candidiasis. Fungi affect the oral cavity (candidiasis stomatitis), rectum (candidiasis proctitis), vagina (“thrush”) and so on. All these diseases, in addition to being extremely unpleasant, accompanied by itching, pain and discharge, are also difficult to treat. After all, yeast-like fungi are one of the most tenacious and rapidly multiplying microorganisms.
Increased candida in feces – causes:
Abuse of carbohydrates, love of sweets;
Long-term antibiotic therapy without antifungal support;
Use of hormonal contraceptives;
Pregnancy;
Diabetes;
emotional stress;
Climate change.
Other opportunistic bacteria
As a result of stool culture, other opportunistic microbes can be detected in the nutrient medium, for example, Klebsiella, hafnia, serrations, proteas, enterobacters, citrobacters or morganellas. All of them are lactose-negative bacteria with varying degrees of potential health hazard. Normally, their total content in the intestine should not exceed 10 to the fourth power CFU / g. If the analysis shows an upward bias, the culprit bacterium is entered on the results sheet as an additional indicator. A significant increase in the number of opportunistic flora (10 to the sixth degree CFU/g or more) requires additional examination and treatment.
The most unpleasant representatives of this group of bacteria:
Klebsiella – antagonists of lactobacilli, cause allergies, constipation, lactase deficiency. Give themselves green and sour smell of stools, the presence of mucus in them (fermentative dyspepsia);
Proteus – lead to the development of constipation, can cause acute intestinal infection with febrile syndrome. When it enters the urinary tract, it provokes cystitis, prostatitis, pyelonephritis.
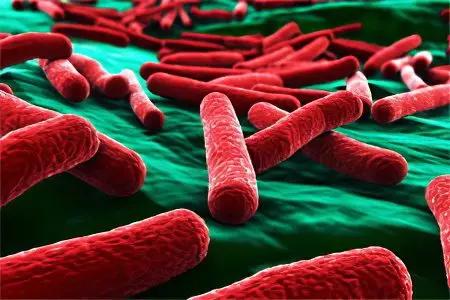
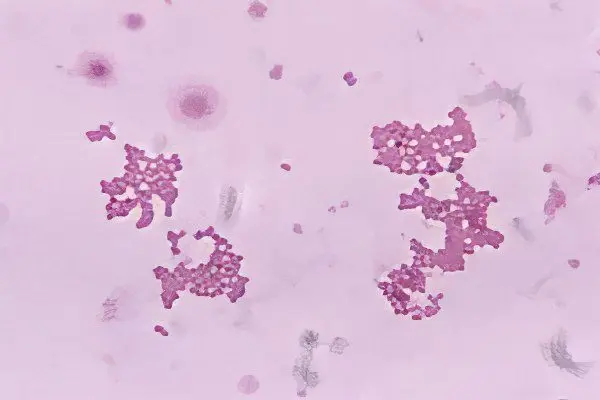
salmonella
Gram-negative facultative anaerobic non-spore-forming bacteria, have the form of thin rods up to 7 microns long, can move with the help of flagella.
Pathogenic for humans, normally, when deciphering the results of the analysis of feces for dysbacteriosis, salmonella should be absent! These microbes cause a serious illness – an acute intestinal infection of the same name.
You can get salmonellosis from a sick person, as well as as a result of eating infected meat, milk, poultry or eggs. It is chicken eggs that are the leading source of the spread of salmonella, so their heat treatment is simply necessary, especially if the dish is offered to a small child. Freezing, salting and smoking meat does not lead to the destruction of salmonella! It also requires long cooking, stewing or baking.
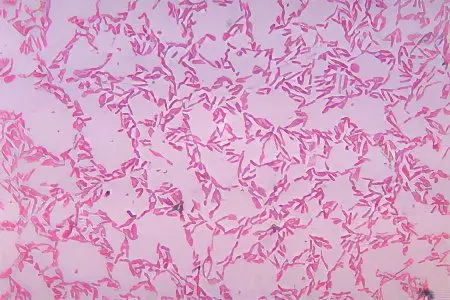
Shigella
Gram-negative, facultative anaerobic, immobile, non-spore-forming bacteria, in appearance they are short (up to 3 microns) rods with rounded ends. Shigella are relatives of Salmonella, they belong to the same family, and are also pathogenic to humans.
In the form with the results of the analysis of feces for dysbacteriosis, there should be a minus opposite shigella – normally, these bacteria are absent! They cause the disease shigellosis, better known as dysentery. This is an acute intestinal infection with high fever, colic, nausea, vomiting and diarrhea.
You can become infected with dysentery through the fecal-oral or contact-household route. Most often, from a sick person, through dirty water, unwashed hands, vegetables, fruits. Flies and cockroaches can also spread shigellosis.
Yersinia
Gram-negative facultative anaerobic rod-shaped bacteria 2-4 microns long, pathogenic for humans, when considering the results of fecal analysis for dysbacteriosis, there should be a dash or abbreviation “neg” in the “Yersinia” column.
These microbes provoke yersiniosis – an acute intestinal infection, the clinical picture of which consists of a febrile syndrome, dyspeptic disorders, abdominal pain and skin rashes.
Yersinia live in the soil, and people usually become infected with them as a result of domestic contact with sick pets (hamsters, rabbits, cats, dogs, parrots) or by eating food and water that the pet has come into contact with for some reason. You can become infected with yersiniosis in the process of caring for livestock (pigs, cows, chickens).
Pseudomonas aeruginosa
Gram-negative obligate aerobic motile bacterium in the form of short (up to 5 microns) straight or curved rods with rounded ends. Scientists disagree as to which group of microorganisms to include Pseudomonas aeruginosa: to opportunistic or pathogenic flora? If we talk about deciphering the results of fecal analysis for dysbacteriosis, then it is better if this bacterium is not sown.
Pseudomonas aeruginosa provokes the development of inflammatory processes in the gastrointestinal tract, urogenital area, respiratory tract, heart, soft tissues. It is the source of 20% of nosocomial infections, 25% of purulent-septic postoperative complications, 35% of all abscesses and phlegmon.
It is easiest to get infected with Pseudomonas aeruginosa from a sick person, by airborne droplets or household contact. It is also transmitted through contaminated food and contaminated water.
Hemolytic Escherichia

Hemolytic or hemolyzing Escherichia is a type of Escherichia coli that is pathogenic for humans. The word “hemolysis”, from which its name comes, means the death of red blood cells – erythrocytes. In the form with the results of the analysis of feces for dysbacteriosis, it should normally be indicated that the patient does not have hemolytic escherichia.
This microorganism causes the development of escherihosis – an acute disease that is accompanied by abdominal pain, nausea, diarrhea, vomiting, fever, headache and dizziness, general weakness and dehydration. All these symptoms are the result of the toxic effects of hemolytic Escherichia coli.
It can be transmitted through contaminated food and water. It is comforting that for a large-scale disease it is necessary to get a fairly large number of Escherichia into the gastrointestinal tract, the disease proceeds quickly (3-6 days) and rarely causes complications. But for elderly debilitated patients and young children, hemolytic E. coli can pose a serious threat!
Staphylococcus aureus
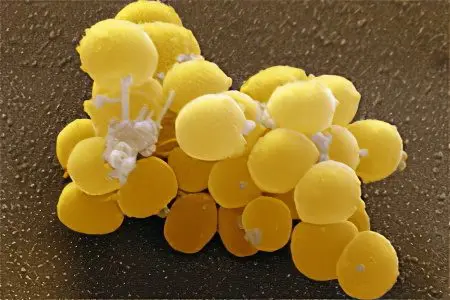
We want to complete our conversation today about deciphering the results of fecal analysis for dysbacteriosis with a description of the most insidious representative of the pathogenic intestinal flora – Staphylococcus aureus. Although, it would be more correct to attribute it to opportunistic bacteria, if only because a quarter of the world’s population acts as its asymptomatic carrier, that is, Staphylococcus aureus can be restrained by the forces of immunity. Some doctors consider the content of this microbe in the studied stool sample at a concentration of 10 to the third degree CFU / g to be acceptable, but there are also experts who consider an exclusively negative indicator to be the norm.
Most people acquire an “intruder” in childhood, as a result of nosocomial spread of Staphylococcus aureus or infection with a bacterium in a preschool educational institution. The first hit of a large amount of the pathogen inside the body of a child or an adult after 4-5 hours causes vivid symptoms of an intestinal infection: nausea, vomiting, abdominal pain, diarrhea with mucus and bloody streaks, dehydration, high fever, weakness, lack of appetite, dizziness sometimes hypotension. It is very difficult to treat the disease – Staphylococcus aureus is extremely resistant to antibacterial drugs. Therapy usually involves the simultaneous normalization of the intestinal microflora and stimulation of the immune system, if required. To avoid such serious problems, it is necessary to carefully observe the rules of personal hygiene, especially when visiting public places, and teach your children to do this. Take care of yourself and be healthy!









