Contents
Amebiasis is an intestinal infection. The disease is characterized by a long course and leads to the formation of ulcers on the large intestine and other organs. Amoeba, as a microorganism, was first discovered by the scientist F. A. Leshem from St. Petersburg. This discovery happened in 1875. The amoeba was found in the stool of a patient who was suffering from bloody diarrhea.
In 1883, R. Koch from Egypt, amoebae were found in purulent liver cavities and in intestinal ulcers. As an independent disease, amebiasis began to be considered only in 1891.
The causative agent of the disease is a protozoan amoeba

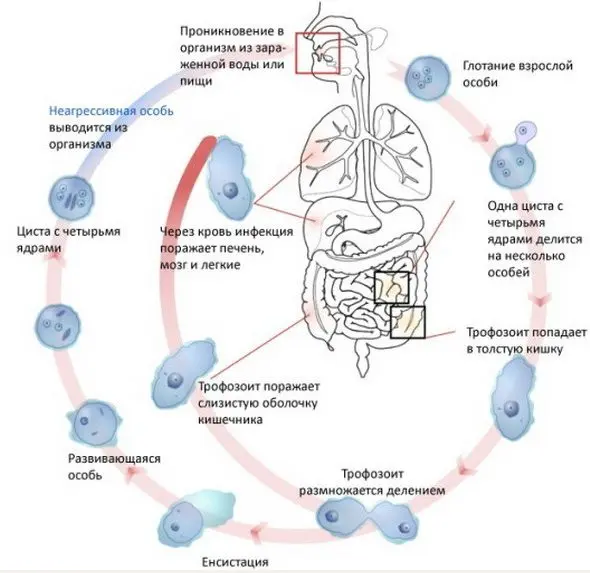
Amebiasis is caused by the simplest microorganism, the amoeba. It goes through 2 stages of the life cycle – the vegetative stage and the cyst stage (at this time the amoeba is at rest).
During the vegetative stage, the amoeba can take a variety of forms:
Fabric form. Such amoeba are very mobile and can penetrate into various environments. During this period, they lead to acute inflammation of the internal organs of their carrier.
Large vegetative form. Such amoebas have the ability to absorb red blood cells.
translucent form. Amoebas lose their mobility. In this form, microorganisms exist in the intestines during the recovery of a person.
In the cyst stage, the amoeba can be represented by two forms:
Precystic the form. Amoeba is characterized by low mobility. In this form, it exists outside the human body. The microorganism retains its activity for several months, if there are favorable conditions for this.
A cyst. Such an amoeba can exist outside the human body for several months. It lives in the soil for 7 days. The amoeba is not afraid of cold, it retains its activity at -20 degrees. The microorganism dies when dried.
Unlike cysts, vegetative forms of amoeba are not stable in the external environment. If the disease has an acute course, luminal and tissue forms of amoebas will be present in the patient’s feces. When a person begins to recover, cysts, translucent and pre-cystic forms are sown in the feces.
The cyst is able to maintain its vital activity outside the human body for a long time. It is represented by a spherical four-core vacuole, which is surrounded by a colorless shell. After the cyst penetrates into the small intestine, a mature amoeba emerges from it, which begins to divide. Each mature amoeba produces 8 new amoebas with one nucleus. All young amoeba have the ability to reproduce. They enter the large intestine in a vegetative form.
Ways of infection
The distributor of amoebiasis is a sick person. It releases various types of amoebas and cysts into the external environment. Moreover, an infected person is contagious after the completion of the acute phase of the disease. It can isolate amoebas for several years. The average number of amoebae that leave a sick person per day is 9000 million. During the acute phase of amoebiasis, a person is not contagious, since he releases vegetative forms of amoebae into the external environment.
People become infected when cysts enter the body. Entry occurs while eating unwashed foods, or with poor hygiene (dirty hand disease). In terms of infection, the danger is unwashed dishes, things, bedding. Carriers of infection can be cockroaches and flies.
Most often, amoebiasis affects men aged 20-50 years. After an infection, immunity is not produced. Amoebiasis is widespread in countries with a humid and hot climate, although infection occurs throughout the world.
Once in the intestine, the cyst transforms into a vegetative form and invades the intestinal wall. In it, it begins to produce substances that destroy the tissues of the organ and lead to the formation of ulcerative defects. They appear from areas of erosions and abscesses, which are represented by nodules. When the nodule is destroyed, vegetative forms of amoebas come out of it, and an ulcer appears in its place. In diameter, each site of ulceration can reach 25 mm.
Ulcers have the ability to merge. The more of them, the higher the probability of damage to the muscular layer of the intestine with its further perforation. This situation is life-threatening, as it leads to the development of peritonitis.
Damage to the vascular walls leads to bleeding of varying intensity. When the intestinal walls begin to heal, this can provoke a narrowing of the lumen of the organ and its obstruction.
If amoebas enter the bloodstream, they are able to spread throughout the body, penetrate the liver, lungs, and brain. If the disease is chronic, then there is a high probability of growth in the intestinal lumen of a tumor-like amoeba. It will be represented by granulation tissue and the body’s own cells.
Amoebiasis forms

There are 3 forms of amoebiasis:
intestinal form.
Extraintestinal form (hepatic, etc.)
Every form.
Intestinal form of the disease
The most common is the intestinal form of the disease. The prodromal period after amoebas enter the body until the first symptoms of the disease appear can last from 7 days to 3 months.
The severity of the symptoms of the disease depends on the severity of its course. They grow gradually.
Patients show the following signs of infection:
An increase in body temperature to subfebrile marks.
Strengthening weakness.
Headache.
Increased fatigue.
Pain in the abdomen that will not be too intense. To a greater extent, a person indicates a feeling of fullness of the intestines.
Abdominal pains intensify, proceed according to the type of contractions. Acute symptoms may persist for up to 7 days. Then comes relief. The disease goes into remission. However, after a few weeks or even months, it may worsen. Such symptoms are characterized by recurrent intestinal amoebiasis.
Sometimes the disease has a continuous course. From time to time, the symptoms fade away, after which they again gain strength. If a person does not receive treatment, then amoebiasis can bother him for many years (up to 10 or more).
The chronic form of infection leads to asthenic syndrome, proteins leave the human body, vitamins are washed out. The tongue is covered with a dense coating, the appetite disappears. The skin becomes dry, facial features are sharpened. On palpation of the abdomen, a person experiences pain.
Intestinal amoebiasis needs to be treated. If therapy is absent, then this threatens the development of severe complications. The heart suffers, the patient develops bradycardia and arrhythmia. The myocardium receives less nutrients.
The nervous system with a long-term current amoebiasis is depleted. A person falls into depression or apathy, he has frequent mood swings, irritability increases.
If the disease is severe, it can lead to complications such as:
Rupture of the intestinal wall.
Intestinal strictures.
Intestinal bleeding.
Pericolitis. The danger is pericolitis, which develops in about 10% of patients. Symptoms of the disease resemble peritonitis. The intestinal walls stick together due to fibrin plaque. They form adhesions and ulcers.
Purulent peritonitis. The accession of a purulent process is accompanied by an increase in pain, an increase in body temperature to feverish levels, vomiting, bloating, and a significant deterioration in well-being.
Tumor in the intestine (ameboma). It grows in the caecum and in the ascending colon. Ameboma often leads to the development of intestinal obstruction.
Intestinal polyps. With amoebiasis, adenomatous neoplasms often form in the intestine.
Prolapse of the rectum.
amoebic appendicitis. This pathology is characterized by a severe course and in 90% of cases leads to death. The complication develops during the acute course of the disease.
Hepatic form of the disease

If amoebas enter the liver, they can provoke the development of hepatitis, or an abscess of the tissues of the organ. The person suffers from intense pain, which will be concentrated in the right hypochondrium.
The doctor during the palpation of the liver notes its increase in size, increased density, pain. Sometimes a person’s skin and mucous membranes turn yellow. Body temperature can reach high levels.
Pain can radiate to the shoulder joint, with a deep breath they become more intense. A change in body position can provoke an attack.
The rise in temperature cannot be called persistent. It may change during the day. The person looks emaciated, his skin is dry, losing its former elasticity. Eyes sunk, cheekbones protrude. In general, the patient looks sickly.
Swelling of the lower extremities is often observed. The abdomen is enlarged. If the disease becomes chronic, then exhaustion will only increase. Liver abscess can be single or multiple. Hepatic amebiasis is a serious disease that often leads to death. If the abscess breaks through, then the pathological masses enter the abdominal cavity, which leads to a clinic of peritonitis. Purulent masses can enter the pleura and lead to the development of pneumonia, or a lung abscess. Such inflammation often acquires a long course.
Other forms of amoebiasis
Together with the blood flow, amoeba are able to spread throughout the body. Sometimes they reach the brain, which leads to symptoms of its defeat. The patient suffers from severe pain, he has convulsions, sensitivity worsens, paralysis or paresis of the limbs may occur.
Amoebas are also able to penetrate the spleen, kidneys, and female genitalia. In these organs, they multiply, which leads to the formation of abscesses in them. Symptoms will be associated with a deterioration in the functioning of a particular system of the human body.
Cutaneous mold disease
When amoebas infect the skin, erosion and ulceration appear on them. The buttocks and perineal area suffer primarily. Ulcerative defects differ in depth, they do not hurt much, but they emit a sharp unpleasant odor.
Diagnosis of amoebiasis

To diagnose amoebiasis, the patient is examined, his complaints are listened to and laboratory tests are prescribed.
According to the results of a clinical blood test, an increase in leukocytes will be noticeable. Moreover, their performance can increase significantly. The ESR also increases.
Feces are examined for the presence of amoebas in it. If there are symptoms of extraintestinal amebiasis, then sputum, pus from abscesses or ulcers should be analyzed.
If translucent forms of amoebae and cysts are not found in the feces, this does not allow excluding the diagnosis of amoebiasis. The fact is that in order to detect protozoa, feces must be handed over to the laboratory no later than 15 minutes after the act of defecation has occurred. The analysis must be repeated several times. When the disease begins to subside, the feces are examined immediately after the patient takes a laxative. If it is impossible to deliver the material to the laboratory immediately after the act of defecation, then it must be preserved. It is examined using Lugol’s solution. Also, amoebas can be cultured on nutrient media, but it will take too long to wait for the results of such a study.
An auxiliary diagnostic method is an immunological analysis. XRF is considered the most effective, followed by the complement fixation reaction. Another way to diagnose is to infect animals with amoeba secretions that live in the laboratory.
Instrumental diagnostic methods may include:
Sigmoidoscopy. During the examination, the doctor examines the condition of the sigmoid and rectum. This method allows you to visualize ulcers, erosions, cysts, polyps and other pathological formations that may appear against the background of amoebiasis.
Organ ultrasoundthat can be attacked by amoebas.
CT scan of the brain, lungs and other internal organs. The study is prescribed in the case when there is a suspicion of the spread of amoebae with blood flow.
Irrigoscopy. This is a method for examining the large intestine. The patient is injected with a contrast agent and several pictures are taken on the x-ray machine.
radioisotope methods. These studies make it possible to distinguish amoebiasis from bacterial lesions of the intestine or other organs.
Microresonance tomography. The method is indicated for those patients who are in a weakened state.
Treatment of amoebiasis

Treatment of amoebiasis involves taking drugs from 3 different groups:
Direct amoebocytes: Yatren, Quiniofon, diyodoquine, tetracycline antibiotics. These drugs are detrimental to the translucent forms of amoebae. They are prescribed to patients with a chronic disease, as well as to recovered people, in order to prevent the development of a relapse of the disease.
Tissue amoebocytes: Emetine, Hingamine, Ambilgar, Dehydroemetine. Medicines of this group destroy amoebae that parasitize in tissues and mucous membranes. They are used to treat an acute form of the disease or for amoebiasis that develops outside the intestines.
Universal amoebocytes: Flagyl, Trichopolum, Tinidazole, Furamid. These drugs allow you to destroy parasite cells from the inside. They act on their proteins, stop the reproduction of amoebae, and also stimulate the formation of radicals that destroy these simple microorganisms.
In addition, patients with amebiasis are prescribed drugs aimed at restoring the intestinal microflora (probiotics). Depending on the developing complications, the patient may be shown drugs to protect the liver, heart, to increase immunity.
If the patient develops anemia, drugs with a high iron content and blood substitutes are prescribed, in rare cases, hemotransfusin. Be sure to take complex vitamins: B vitamins, ascorbic acid.
In a severe form of amoebiasis, infusion therapy is carried out, i.e. reopoliglyukin, glucose-salt solutions are administered intravenously.
Amoebiasis treatment regimens
Treatment of the intestinal form of the disease is carried out according to the following schemes:
Metrics inside 3 times a day for 8-10 days. Dose calculation 30 mg/kg/day.
Tinidazole. Children under 12 years of age are prescribed 50 mg / kg / day, but not more than 2 g per 1 dose. Patients over 12 years old – 2 g / day in 1 dose. The course of treatment lasts 3 days.
Ornidazole. Children under 12 years of age are prescribed 40 mg / kg / day, but not more than 2 g in 2 divided doses. Patients over 12 years of age are prescribed 2 g / day in 2 divided doses. The course of treatment is 3 days.
Secnidazole. Children under 12 years of age are prescribed 30 mg / kg / day in 1 dose. Patients over 12 years of age are prescribed 2 g per day once. The course of treatment is 3 days.
If a patient is diagnosed with an amoebic abscess, then the treatment regimen will be as follows:
Metrics – 30 mg / kg / day in 3 divided doses. The course of treatment is 8-10 days.
Tinidazole. Children under 12 years of age are prescribed 50 mg / kg once a day. Patients over 12 years of age are prescribed 2 g per day once. The course of treatment lasts 5-10 days.
Ornidazole. Children under 12 years of age are prescribed 40 mg / kg / day, but not more than 2 g in 2 divided doses. Patients over 12 years of age are prescribed 2 g / day in 2 divided doses. The course of treatment is 5-10 days.
Secnidazole. Children under 12 years of age are prescribed 30 mg / kg / day in 1 dose. Patients over 12 years of age are prescribed 2 g per day once. The course of treatment is 3 days.
An alternative treatment regimen for amoebic abscess is with the use of dehydroemetin dihydrochloride. Patients are administered 1 mg / kg / day intramuscularly, but not more than 60 mg. The course of treatment is 4-6 days. After completion of therapy with this drug, patients with liver damage are prescribed Chloroquine 600 mg per day for 2 days, after which the dose is reduced to 300 mg per day and taken for another 14-21 days.
In order to completely destroy the protozoa that could remain in the intestinal lumen, after the completion of the chosen treatment regimen, patients are shown taking luminal amoebicides. This can be Etofamide (take it for weeks at 20 mg / kg / day in 2 doses) or Paromomycin (take it for 5-10 days at 1000 mg / day in 2 doses).
Prognosis of the disease
The earlier the disease is detected and treated, the better the prognosis. If there is no therapy, then amoebiasis will progress, leading to severe complications and death.
Prevention
To prevent infection, the following recommendations must be observed:
Timely identify people with infection and prescribe treatment for them.
Put all those who have been ill on dispensary records.
Observe sanitary and hygienic measures: qualitatively process products that are to be eaten, drink clean water, wash hands, etc.









