Contents
Acute pyelonephritis is an inflammatory process that affects the intermediate tissue and the pelvicalyceal system of the kidneys, which has a nonspecific nature.
In urological practice, acute pyelonephritis is the most common inflammatory process affecting the kidneys. It can occur in childhood, a favorable condition for which is the immaturity of the urinary system and a high load on it. Adults also do not fall under the exception; women under the age of 40 are more likely to suffer from the disease.
Doctors separate primary and secondary acute pyelonephritis. The primary occurs due to a violation of the outflow of urine from the kidneys themselves, and the secondary is caused by a violation of its passage due to obstruction of the urinary tract.
Pyelonephritis in the acute phase differs from chronic pyelonephritis:
The course of the inflammatory process in acute pyelonephritis is fast, and in chronic it is slow.
Symptoms in acute illness are pronounced, and in chronic symptoms are often blurred, or completely absent.
Acute pyelonephritis ends with the recovery of the patient, or the transition to the chronic stage.
Chronic pyelonephritis is characterized by frequent relapses of diseases.
Chronic pyelonephritis is more difficult to treat.
Acute pyelonephritis can affect both one and two kidneys. On average, 1% of the world’s population develops pyelonephritis every year. Moreover, it is acute pyelonephritis that accounts for 14% of kidney diseases, and a purulent complication occurs in 1/3 of patients.
Symptoms of acute pyelonephritis
Symptoms of acute pyelonephritis depend on the form of the disease and the stage at which it is located.
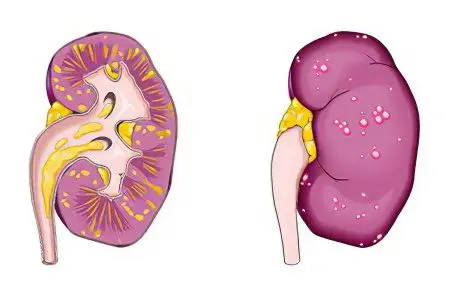
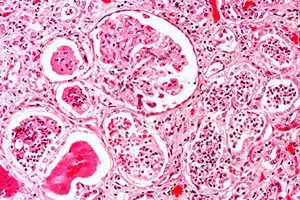
The initial stage of serous inflammation. The kidney increases in size, tenses up, and the fiber located near the film swells. If the disease is started to be treated at this stage, then acute pyelonephritis will be successfully eliminated.
The stage of acute purulent pyelonephritis is divided in turn into three phases: apostematous pyelonephritis, carbuncle and organ abscess. At the beginning, small pustules form in the cortical layer of the kidney, which, if left untreated, merge and form a carbuncle. In the foci of confluence of carbuncles, the parenchyma of the organ melts and an abscess of kidney tissues develops.
Symptoms of non-obstructive pyelonephritis in the acute phase are as follows:
The disease develops very quickly, almost lightning fast. Sometimes it takes a few hours for the patient’s condition to become severe, sometimes it worsens in a day.
A person experiences malaise and weakness, the body temperature rises sharply, reaching a mark of 40 ° C.
Sweating increases, headache appears, heartbeat quickens.
The disease is accompanied by a feeling of nausea and vomiting, arthralgia, diarrhea or constipation.
A person experiences pain in the lumbar region, it radiates to the thigh, back, and abdomen. The nature of the pain is either dull or intense.
As a rule, there are no signs of urination disorders.
There is a not too pronounced decrease in daily diuresis, since the patient loses large volumes of water with sweat.
Urine becomes cloudy, an unpleasant odor emanates from it.
Symptoms of secondary pyelonephritis in the acute phase:
The onset of the disease proceeds according to the type of renal colic, which is associated with urinary tract obstruction.
At the peak of pain, a person’s body temperature rises, up to the development of a fever.
The patient is shivering, thirsty and vomits. (read also: Causes and symptoms of vomiting)
When profuse sweating stops, body temperature sometimes drops to critically low levels, sometimes to normal values. The state of health is somewhat normalized.
An attack of colic returns after a few hours if the obstruction of the urinary tract is not eliminated.
Symptoms of purulent pyelonephritis in the acute stage:
There are persistent pains in the lumbar region.
A person suffers from a hectic type of fever (body temperature fluctuations are 3-4 degrees and occur 2-3 times a day).
An increase in temperature is accompanied by chills.
The muscular walls of the peritoneum tense, the same applies to the lumbar muscles.
When the intoxication of the body reaches a peak, clouding of consciousness and the development of delirium are possible.
Causes of acute pyelonephritis
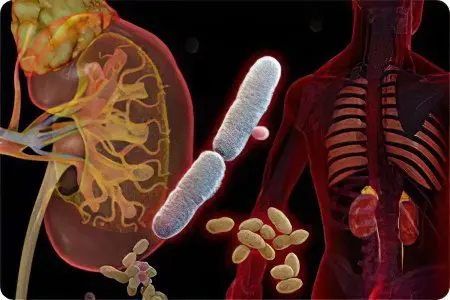
The causes of acute pyelonephritis are the penetration of pathogenic microorganisms into the kidney. In 50% of cases, E. coli becomes this agent, in other cases the disease is provoked by Proteus, Pseudomonas aeruginosa, streptococci, staphylococci, viruses and fungi. Modern urological practice indicates a rare detection of only one causative agent of pyelonephritis. Most often, the disease is caused by the association of several microorganisms. Of particular danger are hospital strains of pathogenic agents in terms of the development of inflammation, since they are very difficult to eliminate.
There are two ways in which pathogens can enter the kidney:
Hematogenous route, in which infection occurs through the bloodstream. This is the most rare cause of inflammation of the kidneys, the hematogenous pathway leads to the disease in only 5% of cases. The primary foci of infection can be: the genitourinary organs, in the presence of inflammation in them (cystitis, adnexitis, prostatitis, etc.), distant organs with sinusitis, bronchitis, caries, tonsillitis, cholecystitis, furunculosis, etc.
The urinogenic route of infection is the most common route of infection to the kidneys. Microorganisms enter them from the lower urinary tract. Another such method of infection is called ascending.
It is worth considering that normally, only the distal urethra can be infected.
In order for the infection to spread further, additional provoking causes or factors are needed, including:
The predominance in the periurethral region and in the area of the perineum of Escherichia coli. This can occur due to intestinal dysbacteriosis, with vaginal dysbiosis in a woman.
Hormonal imbalance.
An increase in the acidic environment of the vagina in women during menopause, which is associated with a lack of estrogen.
The active sex life of a woman and the frequent change of sexual partners facilitates the penetration of infection into the bladder.
Vesicoureteral reflux can cause the development of the disease. At the same time, the retrograde path of urine facilitates the movement of microorganisms from up along the mucous membrane of the urinary tract. This also contributes to increased intrarenal pressure. (read also: Causes and symptoms of intracranial pressure)
Ureteral strictures.
Urolithiasis and blockage of the lumen of the ureter, urethral valve by a stone.
Prostate adenoma and prostate cancer.
Neurogenic bladder.
Subcooling.
Pregnancy.
Diabetes.
ARVI.
Hypovitaminosis and overwork.
The likelihood of acute pyelonephritis increases significantly with a combination of several causes, which happens most often.
Complications and consequences of acute pyelonephritis
Complications and consequences of acute pyelonephritis can be very serious and pose a threat to the life and health of the patient.
The danger may be:
Sepsis.
bacterial shock.
Paranephritis.
Apostematous pyelonephritis.
Kidney carbuncle.
Kidney abscess.
Necrosis of the renal papillae.
Pyonephrosis of renal tissues with their purulent fusion.
Acute kidney failure.
Diagnosis of acute pyelonephritis
Diagnosis of acute pyelonephritis most often does not cause difficulties for a nephrologist. This is primarily due to the presence of clear symptoms of the disease.
Often in the anamnesis of such patients there are chronic diseases or acute purulent inflammations. The clinical picture in acute pyelonephritis is always accompanied by an increase in body temperature to high values and parallel pain in the lumbar region, mostly one-sided. Patients complain of difficulty urinating and changes in the smell and color of urine. It acquires a reddish tint, turbidity is visible in it.
Laboratory tests detect the presence of protein and bacteria in the urine. To determine the type of causative agent of the infection, a bacterial urine culture will be required.
It is also necessary to donate blood for a general analysis. Acute pyelonephritis will be indicated by an increase in ESR and leukocytosis. Identification of the causative agent of infection is possible with the performance of specialized tests.
Plain urography indicates that one kidney is increasing in volume compared to the other.
Excretory urography indicates a pronounced limitation of the mobility of the affected organ, which is noticeable during the orthoprobe. If the patient has apostematous pyelonephritis, then the excretory function noticeably decreases on the part of inflammation, which can be seen during a diagnostic study. A carbuncle or abscess will be indicated by swelling of the contour of the kidney, deformation of the pelvis and calyces as a result of compression.
To assess the structural changes in the kidneys that caused pyelonephritis, it is advisable to perform an ultrasound scan. To assess the concentration capabilities of organs, the Zimnitsky test is used, which will require urine collection.
CT is a method that allows you to exclude or confirm the presence of urolithiasis, as well as to identify possible anatomical abnormalities in the structure of organs.
Treatment of acute pyelonephritis
Non-drug treatment is a prerequisite for the patient’s recovery. It comes down to maintaining sufficient daily diuresis. To do this, the patient must drink liquid in a volume of 2 to 2,5 liters.
To replenish water reserves, you can use fortified decoctions in the form of fruit drinks, which have antiseptic effects. These are cranberries, lingonberries and rose hips. In addition, the use of diuretic fees is shown.
However, only a doctor can recommend drinking plenty of water, since it is contraindicated in heart and pulmonary insufficiency, and in arterial hypertension. If the patient suffers from disorders of carbohydrate metabolism, then the fluid consumed should not contain sugar.
Drug treatment of acute pyelonephritis

If the patient does not have signs indicating urinary tract obstruction, then he is urgently prescribed antibiotic therapy. Its duration can be from 5 days to two weeks. It is preferable to start treatment with parenteral antibiotics. When the symptoms of the acute phase of the disease are stopped, antibacterial drugs are taken orally.
Modern antibacterial agents include:
Fluoroquinolones, which have bactericidal properties. These drugs are not used to treat pregnant women, while breastfeeding, it is not recommended to prescribe them to children and adolescents during a period of active growth.
Drugs from the group of beta-lactams are common aminopenicillins. The therapeutic effect is observed in relation to Escherichia coli, Proteus, enterococci. However, bacteria often develop resistance to drugs of this group and therefore they are recommended to be prescribed for the treatment of pyelonephritis in pregnant women. For all other patients, protected penicillins are used.
Cephalosporins, which are more often than other drugs used by specialists to get rid of pyelonephritis.
Aminoglycosides are prescribed for the treatment of severe nosocomial forms of pyelonephritis, as well as for serious complications of the disease.
In addition to antibiotics, other antimicrobial drugs are also used by doctors, which continue to be taken even after the antibacterial drugs are discontinued. These are nitrofurans: Furazidin, Nitrofurantoin, combined antimicrobial agents: Co-trixomazole, 8-hydroxyquinolines: Nitroxoline. They affect the activity of microbes, effects on the acidity of urine.
Surgical treatment of acute pyelonephritis
When the use of antibacterial agents and other drugs is ineffective, and it is also not possible to restore the patency of the upper urinary tract by installing a catheter, surgical intervention is necessary. It is indicated when the patient’s condition worsens. Operate most often purulent forms of the disease: apostemes and carbuncles of the kidney.
The nature of the operation often remains open until the moment it is performed, the issue is resolved when the extent of the involvement of the kidney in the pathological process is visualized. Its main goal is to prevent the further development of the purulent-inflammatory course of the disease in the kidney, to prevent the transition of the disease to a healthy organ, and to restore the normal outflow of urine.
Physiotherapy
As physiotherapy, methods such as: CMW-therapy, UHF and electrophoresis are used.
It is important to pay attention to the nutritional features of the patient with a predominance of easily digestible protein foods.
Diet for acute pyelonephritis

Diet for acute pyelonephritis implies compliance with strict rules. Thanks to her, it is possible to stop the pain syndrome, correct the acidity of urine. Drinking should be plentiful and at the time of the peak of the disease be at least 2 liters.
When acute symptoms subside, you should switch to a plant-milk diet. Salt in the diet of the patient is limited. It can be consumed no more than 6 g per day, and in case of complicated forms of the disease, it is completely excluded from the diet.
Be sure to have vegetables and fruits with a diuretic effect on the patient’s table: zucchini, melons, watermelons, cucumbers.
Under the absolute ban fall: broths – meat and fish, legumes, smoked meats, marinades, pickles, mushrooms, canned foods, drinks with gases, alcohol, spices and spices (more: what foods are allowed and prohibited in pyelonephritis).
At the stage of recovery, meat products and fish are gradually returned to the patient’s menu. First courses must be vegetarian. Nutrition should be fractional, and food processing methods should be gentle.









