Contents
- What is intestinal obstruction?
- Causes of acute intestinal obstruction
- Symptoms of acute intestinal obstruction
- Stages of acute intestinal obstruction
- Diagnosis of acute intestinal obstruction
- What diseases can be confused with intestinal obstruction?
- Treatment of acute intestinal obstruction
- Complications
- Answers to popular questions
What is intestinal obstruction?
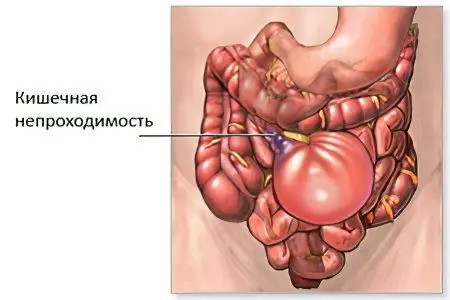
Intestinal obstruction – a pathology in which the process of evacuation of substances from the intestine is disrupted. It is especially characteristic of vegetarians and can be dynamic or mechanical.
At the first suspicion of intestinal obstruction, you should immediately contact the surgeon for help. Only he can make a final diagnosis and advise the necessary treatment. It is very dangerous to stop your choice exclusively on folk methods on your own.
Acute obstruction can cause death of a person, so it is important to know its main symptoms and causes.
Statistics:
After emergency surgery for intestinal obstruction, about 20% of patients die. If the pathology had a severe course, then these figures increase to 40%.
Among all acute conditions requiring surgical treatment, AIO (acute intestinal obstruction) occurs in 8-25% of cases.
If the cause of intestinal obstruction is a tumor neoplasm, then the number of deaths is 40-45%.
When the cause of acute intestinal obstruction is adhesions, death occurs in 70% of cases.
In men, pathology is more common than in women – in 66,4% of cases.
At risk are the elderly, who are 4 times more likely to develop AIO.
Causes of acute intestinal obstruction
Acute intestinal obstruction can be triggered by various reasons. They are divided into predisposing and producing. Predisposing causes contribute to an increase in the mobility of intestinal loops, or to its immobilization. This leads to the fact that the organ occupies the wrong position, and the feces cannot move along it normally.
Predisposing factors can be anatomical or functional.
Anatomical reasons include:
The presence of adhesions in the peritoneal cavity.
Meckel’s diverticulum.
Mesentery too narrow or too long.
The presence of a hole in the mesentery.
The presence of a hernia. The danger is a hernia of the white line of the abdomen, inguinal and femoral hernia, as well as internal protrusions.
Malformations of the organ, for example, mobile caecum, dolichosigma, etc.
Peritoneal pockets.
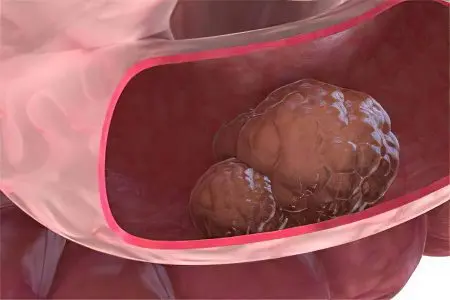
Tumors of the intestines or organs that are in close proximity to it.
Functional causes that can cause acute intestinal obstruction include:
Excessive consumption of food after a long abstinence. If a person has been on a diet for a long time, and then ate a large amount of roughage, the intestines will begin to contract greatly. This can cause intestinal obstruction or “hungry man’s disease” (according to Spasokukotsky).
Colitis of various origins.
Postponed spinal cord injury, TBI.
Psychological trauma.
Stroke.
Dysentery and other conditions that increase intestinal contractility.
Producing causes lead to spasms and paresis of the intestine. An excess of food, a sharp increase in intra-abdominal pressure, physical inactivity (forced bed rest and paralysis) can provoke such a situation.
Symptoms of acute intestinal obstruction

Intestinal obstruction, as a rule, begins with a sharp, growing, cramping pain in the abdomen and is accompanied by nausea and vomiting. Over time, the contents of the intestine begin to enter the stomach, while the vomit has an unpleasant odor characteristic of feces. There is constipation and increased gas formation. Intestinal peristalsis at the initial stage is preserved, it can be observed through the abdominal wall. The abdomen takes on an irregular shape, bloating rapidly increases.
Symptoms of acute intestinal obstruction:
Abdominal pain. It occurs in all patients without exception. At an early stage in the development of pathology, pain proceeds according to the type of contractions. It will be concentrated in the place of the abdominal cavity where the collapse has formed. The pain is present on an ongoing basis, becomes dull, spreads throughout the abdomen. When the pathology reaches its peak, the pain decreases, but this symptom cannot be called favorable.
Nausea and vomiting. These symptoms occur in 60-70% of people. They will be the more intense, the more severe the intestinal obstruction. First, bile will be present in the vomit, and then the contents of the intestine. The masses coming out of the mouth begin to smell like feces. Vomiting does not develop immediately, but after it has begun, its cessation is not expected.
Absence of gases and feces. Even at an early stage in the development of intestinal obstruction, stool will be absent. If the intestinal lumen is not completely blocked, then gases and stools may pass, but partially. At the same time, a person does not experience relief, he does not have the feeling that the intestines have completely cleared.
Bloating, changing its natural outlines. Most often, this symptom characterizes otrutsionny intestinal obstruction. If the blockage occurs in the area of the small intestine, then the peritoneum will be swollen evenly. With damage to the large intestine, the abdomen acquires asymmetric features and swells in one of the areas.
Forced position of the body – the person lies down and pulls his knees to his stomach. The patient cannot lie quietly, he constantly turns over, as he is pursued by severe pain.
The general well-being of a person at an early stage of the development of pathology can be called satisfactory. However, if he has a strangulation of the intestine, then the state of health worsens already in the first few hours from the development of the disorder.
The level of blood pressure falls, and the pulse rises, which indicates the development of a shock state.
The tongue becomes dry, a yellow coating forms on it, and an unpleasant odor comes from the mouth. If the blockage occurs in the area of the small intestine, then the smell will have a fecal tinge. The terminal stage of the development of pathology leads to the appearance of cracks in the tongue, after which ulcers form on it. This indicates severe poisoning of the body, its dehydration and developing peritonitis.
When the patient goes to the doctor, the doctor notes the following clinical picture:
Palpation of the peritoneum gives a person painful sensations. With deep probing, a tumor or intussusceptum can be determined. Also, the doctor can palpate the hernia. The wall of the peritoneum will be stretched, but the abdominal muscles are not tense. The doctor also notes an intense contraction of the intestine.
Tevenard sign. When pressing on the root of the mesentery of the small intestine (it is located 2 cm below the umbilical fossa), a person experiences pain.
Val’s sign. On palpation of the anterior wall of the abdomen, the adductor loop is well palpated. Its contour can be visualized.
Anstutz syndrome. In the right iliac region, the abdomen will be swollen.
Palpation of the intussusceptum. It is defined in the region of the ileocecal angle and has a shape resembling a sausage.
Shlange’s symptom. Even without special devices, you can notice how the patient’s stomach swells from gases.
Sklyarov’s symptom. If you shake the anterior wall of the peritoneum with your hand, you can feel its seething.
Listening to the abdomen. The doctor will hear a loud noise. If the pathology has already provoked the death of the intestinal walls, then the seething stops, giving way to silence.
Loteison sign. When listening to the anterior wall of the peritoneum, heart and respiratory murmurs can be heard.
Syndrome of the Obukhov hospital (Grekov’s sign). The anus is dilated, as is the rectum, but no stool is observed there. This symptom is characteristic of volvulus.
Kivul’s symptom. When tapping the anterior wall of the abdomen, a ringing can be heard. If it has a metallic tint, then indicate a symptom of the balloon (Kivul’s symptom). If you tap the side of the abdomen, the sound will be somewhat muffled.
Tzege-Manteifel symptom. It is characterized by the fact that when performing an enema, more than 1,5 liters of fluid does not enter the intestine. Such a symptom is diagnosed with volvulus of the sigmoid colon.
Mondor syndrome. On palpation of the rectum, you can feel the tumor in it and visualize the feces, which will have a crimson color.
Typical manifestations of invagination are:
Severe pain in the abdomen according to the type of attack (Tiliyaks symptom).
False urge to defecate and palpation of the formation in the peritoneal cavity (Rush symptom).
Bleeding from the anus (Crovele’s symptom).
Setting an enema leads to the fact that the outgoing contents resemble the appearance of meat slops.
Stages of acute intestinal obstruction

Pathology, despite the acute course, has a certain staging.
Experts distinguish 3 phases:
1 phase – reactive
The duration of the reactive phase is 10-16 hours. During this period, a person experiences intense pain like contractions. At first they are paroxysmal, with periods of calm, but later become permanent. Often the pain is so severe that the person goes into shock. Doctors call the reactive phase the “Jelius cry.”
When the reactive phase has just manifested, intervals without pain will be frequent, at which time the patient’s well-being is normal. However, with infringement of the intestine, light gaps are not observed. Pain changes from moderate to severe. High intestinal obstruction is accompanied by nausea and vomiting. With low intestinal obstruction, gas formation increases, there is no stool.
The pain is visceral, radiates to other organs, develops against a background of spasm, in which intramural nerve plexuses are irritated. In the future, the motor function of the intestine is depleted. The intestines become edematous, greatly stretched. As the swelling increases, the pain becomes constant and intense. There are no periods of enlightenment.
2 phase — intoxication
After 12-36 hours, a toxic phase develops, in which paresis of the organ is observed. The pain becomes constant, the intestines stop contracting, the stomach swells, takes on an irregular shape.
A person develops vomiting, it is plentiful, it is impossible to stop it. The intestines during this period will be full, as well as the stomach.
A person refuses water, as he is constantly sick. This leads to dehydration of the body, minerals, electrolytes, enzymes are removed from it. The face becomes like a mask (the face of Hippocrates), the oral mucosa dries up, while the patient himself is very thirsty. He has severe heartburn. Neither feces nor gases come out.
During this period, Valya’s symptom, Sklyarov’s symptom, Kivul’s symptom, and peritoneal irritation symptom appear. The function of lists suffers. Since a lot of fluid accumulates in the intestines, it begins to seep through its walls. This becomes the first step towards the development of inflammation of the peritoneum.
3 phase – terminal
After 36 hours, the final stage of the pathology develops. In this case, all organs are affected. The person begins to breathe rapidly, the body temperature rises to feverish levels, there is no urination. The abdomen is no longer protruding forward, blood pressure drops, and the pulse becomes very frequent, but weak.
From time to time, the patient experiences vomiting, from which the smell of feces emanates. Then the patient develops blood poisoning, insufficiency of internal organs and death occurs.
Diagnosis of acute intestinal obstruction

If a person has symptoms of acute intestinal failure, you should not hesitate to contact the doctor. The surgeon who examines the patient and listens to his complaints is engaged in identifying the violation.
Laboratory methods
In addition to external examination and palpation of the abdominal cavity, the doctor directs the patient to undergo laboratory tests, including:
General blood analysis. A shift of the leukocyte formula to the left, an increase in ESR and hematocrit are detected. This is due to the increasing dehydration of the body, against which the blood becomes thick.
Donating blood for biochemical analysis. The analysis will increase the level of nitrogen, urea, glucose. At the same time, the values of potassium and sodium, calcium, chloride and proteins fall.
Urine becomes cloudy and dark in color. The laboratory assistant detects erythrocytes and albumins in it.
The coagulogram shows blood clotting, the prothrombin index increases, the blood clotting time becomes shorter.
X-ray
X-ray of the intestine is the most accessible and very informative method for detecting intestinal obstruction. It has a low cost and is also easy to implement. The procedure is performed using barium as a contrast medium. Separately, an x-ray of the intestine and an x-ray of the abdominal cavity are performed. If it is not possible to clarify the diagnosis, then resort to irrigoscopy or intestinoscopy. These studies allow you to assess the condition of different parts of the intestine. Alternatively, endoscopy of the lower intestine is performed.
During the fluoroscopy, the patient should lie (on the side or on the back) or stand.
The characteristic picture that the doctor visualizes:
Cloiber bowls. This symptom is accumulations of gases that look like inverted bowls. It is this clinical sign that is one of the first to be detected. When the intestines are cut off, Kloiber’s bowls are visible on the x-ray after 5 hours, and when the organ is strangulated, after an hour. The bowls can be multiple, they can be layered one on top of the other, so they resemble the look of a staircase.
Intestinal arcades. They are formed in the small intestine. Due to pathology, it swells, overfilled with gases. In the lower sections of the arcades, horizontal liquid levels are noticeable.
A symptom of featheriness. It develops with high obstruction, since in this case the small intestine is greatly stretched. It is its walls that form folds. In the picture, it looks like a spring that has been stretched.
X-ray with contrast involves the absorption of 50 ml of barium suspension by the patient. Then the doctor takes a picture of the gastrointestinal tract. They are made several, at certain intervals of time. If barium remains in the intestine for a long time (longer than 4 hours), then this may be a sign of an obstruction.
Depending on where the intestinal obstruction has developed, the x-ray picture will be as follows:
With obstruction in the small intestine, the Kloiber bowls will be small. The width of the liquid level is greater than the height of the gas. Regardless of the section of the intestine, the levels of fluid in them will be the same. The rosary shows spirals and arcades, represented by the mucous membrane of the organ.
With obstruction of the jejunum, fluid levels will be located in the epigastric region and in the region of the right hypochondrium.
If the distal ileum is obstructed, fluid levels will be located in the center of the abdomen.
In colonic obstruction, fluid levels are located on the sides of the abdomen, but they are much less than in the case of blockage of the small intestine.
With dynamic intestinal obstruction, fluid levels are visualized in the small intestine and colon.
If the doctor assumes that the patient develops obstruction of the large intestine, then he prescribes sigmoidoscopy and colonoscopy. These diagnostic techniques allow you to determine the cause of the violation and identify a tumor, foreign bodies or fecal blockages.
What diseases can be confused with intestinal obstruction?

Symptoms of intestinal obstruction may resemble signs of other diseases. Therefore, it is possible to confuse obstruction with such violations as:
Acute appendicitis. With this disease, severe abdominal pain also occurs, vomiting and constipation may develop. However, with appendicitis, pain originates in the epigastric region, moving to the right iliac region. With obstruction, the pain proceeds according to the type of contractions, it is intense, replaced by painless periods. Such intense contraction of the intestine does not occur with appendicitis. If a general blood test for both pathologies will indicate the presence of inflammation, then there are no signs of obstruction when performing an x-ray of the intestine.
Perforated stomach ulcer. The disease develops as suddenly as intestinal obstruction, the patient has no stools and gases, the stomach hurts a lot. If there is a perforation, then the person will feel very bad. The anterior abdominal wall is very tense, does not take part in breathing. If you try to palpate the intestines, then the person will feel severe pain. With obstruction, the organ, on the contrary, is greatly reduced, it is possible to palpate an enlarged loop. With an ulcer, a person does not develop vomiting, the intestines do not contract. During the X-ray, Kloiber’s cups are not detected, but free gas is visible in the peritoneal cavity.
Acute inflammation of the gallbladder. A person has intense pain, he is sick, his stomach swells. However, the pain will be concentrated in the right side, radiating to the shoulder and shoulder blade. With obstruction, it will not be possible to clearly limit the location of the pain. If the region of the right hypochondrium is palpated, then tense muscles can be detected in a patient with cholecystitis, while the contractile activity of the intestine does not increase, pathological sounds are not heard. With inflammation of the gallbladder, body temperature rises, jaundice develops.
Acute inflammation of the pancreas. Pain manifests suddenly, vomiting occurs several times in a row, gases do not go away, the stomach is swollen, the intestines are in a state of paresis. The stomach hurts in the upper part, the pain encircles the body. With intestinal obstruction, the pain proceeds according to the type of contractions. If you palpate the abdomen of a patient with pancreatitis, you can feel the swollen colon. In addition, bile will be present in the vomit. After some time, the gases will begin to move away, a chair will appear. In the blood test, the level of diastase increases.
Myocardial infarction, accompanied by abdominal syndrome. A patient with a heart attack has a swollen stomach, severe pains appear in its upper part, weakness increases. A person is sick, vomiting may open, there are no stools and gases. However, additional signs that indicate a heart attack are: hypotension, deafness of heart tones, percussion expansion of the borders of the heart, the abdomen does not become asymmetric, the intestine does not contract much, and noise does not appear. To clarify the diagnosis, you need to perform an electrocardiogram.
Renal failure. Similar signs are: intense pain by the type of contractions, bloating, lack of stools and gases, increased anxiety of the patient. Distinctive characteristics of renal colic: pain radiates to the genitals, to the lower back, urine is delayed, a person can urinate with difficulty, there is blood in the urine. Stones are found in the kidneys and ureters with the help of X-rays.
Pneumonia concentrated in the lower lobes of the lungs. Similar symptoms: abdominal muscle tension, abdominal pain. Distinctive characteristics of pneumonia: pinkness of the cheeks, shallow breathing, shortness of breath, chest pain. If you listen to the lungs, you can hear wheezing, crepitations, noises. X-ray helps to make the correct diagnosis.
Treatment of acute intestinal obstruction

If a person develops symptoms that indicate intestinal obstruction, they should be taken to a medical facility as soon as possible. Until such time as the patient is examined by a doctor, he should not do an enema, it is forbidden to take laxatives, painkillers or perform gastric lavage. Treatment can be reduced to both medications and surgery. It all depends on the characteristics of the course of the disease. With dynamic obstruction, there is the possibility of medical correction, and with mechanical blockage of the intestine, it will not be possible to do without the help of a surgeon. Often, to save the life of the patient, the operation is performed on an emergency basis.
When obstruction has just begun to develop, it is difficult to identify its form. Therefore, the doctor postpones the intervention for several hours. If taking medications does not lead to an improvement in well-being, then the patient is sent to the surgical table. Provided that the patient has already been diagnosed with peritonitis or intestinal strangulation, the operation is performed immediately.
Drug correction often allows to overcome coprostasis, as well as to cope with obstruction against the background of a neoplasm in the intestine.
Medical correction
Reducing the intensity of pain, influencing the contraction of the intestine. Pararenal novocaine blockade is performed to reduce pain. Antispasmodics (Atropine, Spazgan, Drotaverine) are administered intravenously. If a patient is diagnosed with intestinal paresis, then Neostigmine, hypertonic sodium chloride solution is prescribed to eliminate it, and an enema is performed.
Decompression of the digestive tract. The contents of the stomach should be removed using a probe and a siphon enema, through which 10 liters of water are injected. Such measures can be performed only on the condition that the patient has not developed peritonitis. If chyme is found in the stomach, this indicates a severe course of intestinal obstruction. Also, the volume of injected fluid allows you to make an assumption about the level of obstruction. Carrying out decompression makes it possible to normalize the contractility of the intestine and improve microcirculation in its walls.
Prevention or elimination of dehydration. Patients with intestinal obstruction are prescribed infusion therapy. Patients are given Ringer’s solution, glucose, insulin, potassium solution. The volumes of injected solutions are large and cannot be less than 3 liters. Soda is prescribed to patients with metabolic acidosis. During infusion therapy, it is necessary to control pressure and urination. The patient is placed a catheter in the bladder and in the subclavian vein.
Normalization of the blood supply to the digestive organs. For this purpose, albumin, plasma, protein, reopoliglyukin, pentoxifylline, amino acids are used. If there are indications, the patient is prescribed cardiotropes. If the patient starts the process of passing gases, stool appears and the pain disappears, then this is a good sign. If after 2-3 hours the person’s health does not improve, he is prepared for surgery.
Operative intervention

If a patient develops a mechanical blockage of the intestine, then surgery is required in 95% of cases. The remaining 4% of patients do not undergo it due to the fact that they are in a serious condition. Another 1% of patients simply do not seek medical help and die.
Contraindications to surgery for mechanical blockage of the intestine are only the agony and pre-agony of the patient.
Indications for surgery:
developing peritonitis.
Intoxication and dehydration of the body, which corresponds to the 2nd phase of obstruction.
Signs indicating intestinal strangulation.
Measures to prepare the patient for intervention:
Probe placement in the stomach.
The introduction of drugs that will ensure the functioning of the circulatory and respiratory systems.
Carrying out massive infusion therapy.
The patient is placed a catheter into the bladder, into the stomach and into the central vein. Anesthesia is done endotracheally, the operation is laparotomy with a median incision. If the patient’s obstruction is due to infringement of the hernia, then spinal anesthesia can be performed.
Goals pursued by the surgeon:
Determining the type of obstruction with an examination of the abdominal organs.
Elimination of the cause that provoked the blockage. Adhesions or hernia gates are dissected, when the intestines are twisted or when a node is formed, they are eliminated. Disinvagination is also carried out, or a resection of part of the affected area is planned.
Assessment of the condition of the intestine and its possibility of further functioning. If the organ has not died, then it will have a burgundy or blue color, its mesentery is smooth in some of its zones, hemorrhages are visible. The vessels continue to pulsate, there are no blood clots. The intestine reacts to the effect of warm saline with hyperemia, increased pulsation and contractions. Removal of the organ is required in case of formation of blood clots in the vessels, if it becomes black or dark blue, the mesentery will be dull and covered with hemorrhages. The intestine does not respond to treatment with a warm solution.
Removal of the affected area. The part of the organ that has undergone necrosis, as well as the intestine at a distance of 40 cm from the dying zone, is subject to removal. Then an anastomosis is performed.
Unloading. When the organ loops have been overstretched, bowel decompression is performed using a nasogastric intubation of the small intestine with a tube. Drainage is performed through an enterostomy or cecostomy.
Drainage and sanitation of the peritoneum. The abdominal cavity is washed with special compounds, dried. Drainage is removed through the anterior abdominal wall.
Period after surgery

If the operation was successful, then the patient is placed in the intensive care unit. There he must spend at least 3 days.
The main directions of treatment and care:
Prevention of dehydration, intoxication and infection of the body.
Elimination of violations of the respiratory and cardiovascular systems.
The use of electrolytes to normalize the acid-base environment.
Improvement of rheological parameters of blood.
Preventing the formation of blood clots. For this purpose, Fraxiparine is used.
To strengthen the body, vitamins and immunomodulators are administered.
To prevent paralysis of the intestine, its work is supported with the help of enemas, Prozerin, Cerucal, electrical stimulation, etc.
In the first 3 days, the person should be in the intensive care unit. He is given a percussion massage of the sternum, and breathing exercises are performed. This is necessary for the normalization of the respiratory system.
Get the patient out of bed as soon as possible. This is done so that the intestines begin to contract and stagnation does not develop. It is recommended for the patient to get up for 2-3 days, if there are no contraindications.
The first 3 days a person receives parenteral nutrition. It is important to control his pulse, respiratory rate, and the quality of the discharge from the drainage. In the same period, he receives antibiotics and anti-inflammatory drugs.
On the 4-7th day, the patient is transferred to the general ward. There he must observe half-bed rest. The probe is removed from the stomach. From now on, a person should receive food as usual, but it is served in a semi-liquid and grated form (table 1A).
The bandage is changed for 2 days, the drainage is removed on the 4th day, if there is no discharge from it.
In order not to separate the seams, the patient should use a bandage. From day 5, you need to start doing gymnastics under the supervision of a doctor. The patient continues to receive vitamins, antibiotics, and immunity stimulants. The menu is slowly expanding.
On the 8th-10th day after the operation, a person is transferred to table No. 15. He is already allowed to leave the room.
The stitches will be removed on day 9-10. If no complications develop, the patient is discharged.
In the next 3 months, a person will need to follow a strict menu, give up vegetables that stimulate gas formation, pickled and salty foods, fatty foods and semi-finished products.
Complications

The postoperative period is associated with the risk of the following complications:
Necrosis of the intestinal loop. In this case, a second operation is performed, the affected area is removed, anastomosis is applied, or the stoma is removed.
Bleeding. A second laparotomy is required during which the source of bleeding is eliminated.
Failure of the sutures of the intestinal anastomosis. At the same time, a relaparotomy is performed, an unnatural anus is created, and drainage is removed.
Interintestinal abscess. Perform relaparotomy and debridement of the abscess.
Intestinal fistula. Perform conservative therapy, with the treatment of the fistula with disinfecting ointments and pastes. In the future, the loop with the fistula must be removed by performing intestinal intubation.
The formation of adhesions. Perform relaparotomy with fistula dilution, intestinal intubation.
Answers to popular questions
Is it possible to make a prognosis for acute intestinal obstruction? The sooner the patient is helped, the more favorable it is. Concomitant diseases, as well as the age of the patient, are important. For the elderly and debilitated people, the prognosis worsens. If the operation was performed in the first 6 hours from the development of obstruction, then the patient can most often be saved.
If the obstruction develops in a pregnant woman, what is the prognosis? The period of gestation is an additional risk factor for the development of intestinal obstruction. Most often it happens in the 2nd and 3rd trimester of pregnancy, less often in the 1st trimester. In 25-50% of cases, pathology leads to the death of a woman, and a child is born dead in 60-75% of cases. However, provided that the operation was performed in the first 3 hours from the manifestation of obstruction, the death of the patient occurs only in 5% of cases.
What is chronic intestinal obstruction? It develops against the background of the presence of adhesions in the abdominal cavity, or with a tumor that cannot be removed. The patient is prescribed medication. If there is no effect, then an operation is performed. At the same time, each intervention is associated with the risk of the formation of new adhesions. Alternatively, a colostomy may be formed.










hewlii hawdartai yumaa tegsen tvgjrel vvssen bn yaah estoi we yaaralrai zowolgoo ogch tuslaach