Contents
In line with its mission, the Editorial Board of MedTvoiLokony makes every effort to provide reliable medical content supported by the latest scientific knowledge. The additional flag “Checked Content” indicates that the article has been reviewed by or written directly by a physician. This two-step verification: a medical journalist and a doctor allows us to provide the highest quality content in line with current medical knowledge.
Our commitment in this area has been appreciated, among others, by by the Association of Journalists for Health, which awarded the Editorial Board of MedTvoiLokony with the honorary title of the Great Educator.
An abdominal aortic aneurysm may present with pain in the abdomen and back in the sacrum area, but it may also be asymptomatic at all. In both cases, it is a life-threatening condition.
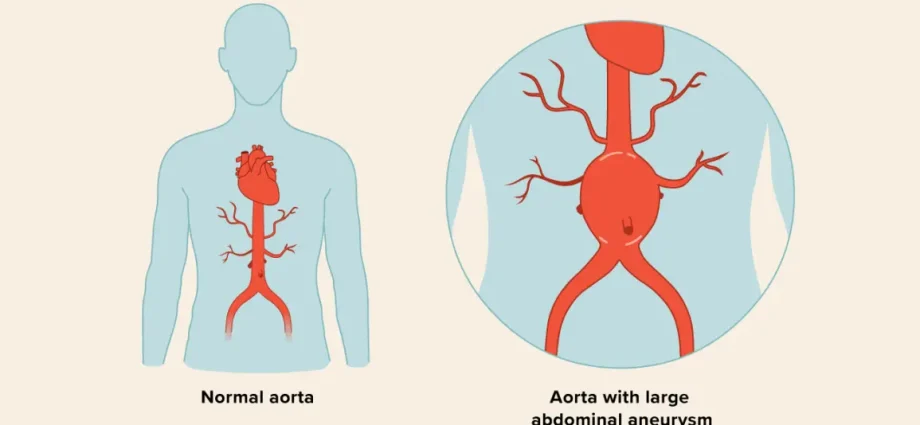
Abdominal aortic aneurysm (TAB for short) is one of the largest arteries that drains blood from the heart. The aorta runs through the chest and abdominal cavity and splits into two iliac arteries that run down the legs. An aneurysm is formed when the aorta in a given place increases its diameter by 50%, i.e. it is more than 3 cm. Aortic aneurysm can occur in any part of the aorta, but most often it is located in the infrarenal part.
Abdominal aortic aneurysm risk groups
Statistically, an abdominal aortic aneurysm occurs in 60 out of 100 people, which is rare. However, statistical data show that it is 3 to 8 times more common in men: 3% aged 60–65, 6% aged 65–74 and as much as 9% over 75 years of age. In recent years, there has also been a steadily increasing incidence, which is confirmed by both post-mortem examinations and the increased detection of this disease. We live longer and longer, but the older we get, the more often we fall ill. We also have better and better medical equipment to help detect and diagnose aneurysms. Finally, in the 90s, reports of a familial occurrence of aneurysms appeared, indicating the possibility of genetic transmission of the predisposition to this disease. In addition, aneurysms like to appear in several places. Often common iliac artery aneurysms are accompanied, for example, by aortic aneurysms. In 30–50% of cases, these are also bilateral aneurysms.
Causes of the abdominal aortic aneurysm
In addition to the unexplored genetic factors, there are also other causes of this disease. The most frequently mentioned are the degeneration and weakening of the lining of the arterial walls, which arise as a result of persistent chronic hypertension and elevated blood cholesterol levels. It is known that cholesterol likes to deposit on the walls of arteries in the form of atherosclerotic plaques, which causes constriction of the vessels. And this results in a further rise in blood pressure and an overload of the walls of the vessels, which, like an inflated balloon, finally begin to burst at their weakest point. In this way, the cholesterol-hypertensive circle closes.
Studies also show that aneurysms are more common in smokers, overweight and obese people, and in patients with severe obstructive pulmonary disease and after heart attacks.
Diagnosis of an abdominal aortic aneurysm
The number of diagnosed and operated aneurysms of the abdominal aorta is constantly growing, as ultrasound screening tests are performed more and more often. Such tests should be performed in all people over 65 years of age, and in the younger age group in people with a family history of aortic aneurysm, and in patients with atypical back or spine pain in whom degenerative changes have been excluded.
Scientific research into the presence of family and genetic predisposition is moving towards developing laboratory tests to identify putative candidates who may develop an aneurysm. However, no standards have yet been developed that would allow easy and unambiguous diagnosis of aneurysms. The reasons for this fact include different types of them, which – depending on the place of origin, size and type – may give very different symptoms or cause no symptoms at all.
So if the patient says that he feels like a pulsating tumor in his abdomen, his abdomen and his back hurt a lot in the sacral area, the doctor has the right to suspect an abdominal aortic aneurysm.
Generally, aneurysms can be divided into: asymptomatic, symptomatic and ruptured due to their symptoms. Due to the genesis, structure and frequency of occurrence, there are also other types of aneurysms, e.g. dissecting, inflammatory, embolizing, true, and infected aneurysms.
The hallmark of a dissecting aneurysm is aortic dissection, which creates two blood flow channels that communicate with each other. The channel produced is located in the outer mid-membrane portion and has a thin outer wall susceptible to rupture. If the dissection is chronic, it forms slowly and gives the patient time to respond. If it is acute – it arises suddenly and threatens the patient’s life. Then the sooner the patient finds medical help, the greater the chance of saving him. Statistics show that mortality increases by 1-2% in each subsequent hour in untreated people. That is why American standards require that the time from diagnosis to starting treatment should be limited to 30 minutes. Unfortunately, we are far from reaching these standards in Poland. Even if an ambulance does manage to arrive, in severe cases of cracks, it happens that patients die during transport to the hospital.
Dangerous cracks
When it comes to aneurysm rupture, any scenario of this is dangerous. However, several variants are possible.
And so: if the inner aortic membrane ruptures, the blood will either squeeze into the medial membrane, break another membrane and come out into the retroperitoneal space, or it will hollow a new channel in the inner membrane, it will return to the inside of the vessel and flow in harmony. with the physiology of the body, or getting into the peritoneum.
In the first case, there is a chance of saving the patient’s life thanks to the phenomenon of autotamponade at the rupture site, which occurs when the pressure in the tight retroperitoneal space exceeds the pressure in the aorta. A typical symptom of retroperitoneal aneurysm rupture is a hematoma of the scrotum and / or around the anus. Such a rupture may last for days or weeks before another hemorrhage occurs. This gives the patient time to seek medical attention. Most often, however, the second hemorrhage occurs after a few or several hours, so each patient should immediately go to the hospital when hematomas in the anus or scrotum are noticed.
If additional blood circulation is created inside the aorta between its stratified membranes, an intramural hematoma is formed, which is life-threatening, even though apparently nothing happened because the blood returned to the inside of the vessel.
It is worst when the aneurysm is perforated into the peritoneal cavity. There is then severe abdominal pain and rapidly increasing symptoms of hemorrhagic shock, which practically do not give the patient time to call for help. It is then that death often occurs while the patient is transported to the hospital.
Other, less frequent, routes of aneurysm perforation are possible. It can rupture, for example, into the duodenum (gastrointestinal bleeding) or into the inferior vena cava, which gives non-specific symptoms: abdominal pain, swelling of the scrotum and lower limbs with bruising of the skin, widening of the superficial veins of the abdomen and lower extremities, rarely rectal bleeding and hematuria.
Methods of treating an abdominal aortic aneurysm
The treatments for aneurysms depend on the size and location of the aneurysm, and therefore the potential risk of an aneurysm rupturing. As a rule, aortic aneurysms smaller than 4 cm in diameter are not operated on. In the initial stage of the disease, only pharmacological treatment with beta-blockers is used, which slows down the rate of growth of thoracic aortic aneurysms. However, for patients with an abdominal aortic aneurysm, the data are inconclusive: a beta-blocker may be considered, but there is no guarantee that it will slow down the aneurysm enlargement.
The next stage of symptomatic treatment of an aneurysm is endovascular treatment, which involves the implantation of a stent graft (stent) by the lumen of the artery into the aorta. It is a small “spring”, most often made of 316 LVM steel or a chrome-cobalt alloy, coated with Dacron, placed inside a blood vessel to expand the vessel from the inside. Dakron (a plastic substance composed of polyethylene terephthalate) is distinguished by its mechanical memory – after being stretched in an appropriate segment, it adjusts to the size of the aorta and “remembers” the given shape. Vascular stents can be balloon-expanded and self-expanding. They are most often introduced into the aorta with a probe through the femoral artery and then fixed at the site of the aneurysm. However, despite a shorter hospitalization time and a faster return to normal activity after stent graft implantation, in the light of today’s studies, it seems that such a procedure – compared to open surgery, does not ensure longer survival taking into account the quality of life.
Finally, the last stage of treatment of endangered or already ruptured aortic aneurysms is excision of the aneurysm and prosthesis of the removed section with a Dacron prosthesis with traditional opening of the chest or abdomen. In the case of dissecting aneurysms, also sewing the walls of the artery or cutting the septum separating the two dissection channels are also used.
What else is worth knowing? The occurrence of an aneurysm larger than 4 cm is not an absolute indication for surgery, as statistically rupture is less frequent than the operative mortality (for most patients with aneurysm diameter up to 5,5 cm). Operations of this type are technically very difficult and can be associated with complications. This is due to the fact that many tiny vessels depart from the aorta, which need to be sewn together precisely in order to prevent the patient, for example, from paralysis of the limbs.
The most common types of an abdominal aortic aneurysm
- Asymptomatic aneurysm
It does not give any characteristic symptoms. Occasionally, patients report a feeling of fullness after eating a meal or painful abdominal pain that is difficult to locate.
- Symptomatic aneurysm
It most often causes pain in the sacro-lumbar region (often imitating sciatica), in the lower abdomen, and radiates to the thighs, bladder, perineum and testes. When it reaches large size, swelling of one or both limbs appears, as well as proteinuria and hematuria. 20% of patients experience weight loss. An aneurysm measuring 5 cm can be detected in 80% of cases by palpation of the abdomen.
- A ruptured aneurysm
The likelihood of an aneurysm perforation increases with the diameter of the aneurysm. Those with a diameter of up to 5 cm break in 5–23% of patients, larger than 7 cm – in 60–80% of cases within a year. It is manifested by sudden pain in the lumbar region radiating towards the lower abdomen and perineum. Internal hemorrhage and shock appear. A typical symptom of a retroperitoneal aneurysm rupture is a hematoma of the scrotum and / or around the anus, appearing several hours after rupture.
Each patient should go to the hospital immediately when he notices hematomas in the area of the anus or scrotum.
Also read: Insidious aneurysms










আমি ২ মাস ধরে আমার পেটের নাবির বাম পাসে একটু ফোলা চাপ দিলে লাপাই যেমন হার্ট মত সাথে বাম পাসে অন্ডকোষ ব্যথা করে আমি আন্তাসোনুগ্রাম পরিক্ষা করি ডক্টর বললেন রগের সমস্যা ঔষধ খেয়েছি কিছু হয়নি এখন আরু বেড়ে যাই একটাকি এই রুগ সাথে বাম পাসের গলায় টনসিল মত ফুলে গেছে এখন কি করব