Contents
- When the placenta is inserted low
- What is an anterior placenta, posterior placenta, fundal placenta?
- When the placenta is infected
- When the placenta has a funny shape
- When the placenta comes off too soon
- Placenta accreta: when the placenta implants poorly
- When the placenta grows abnormally
- In video: Terms related to the placenta
When the placenta is inserted low
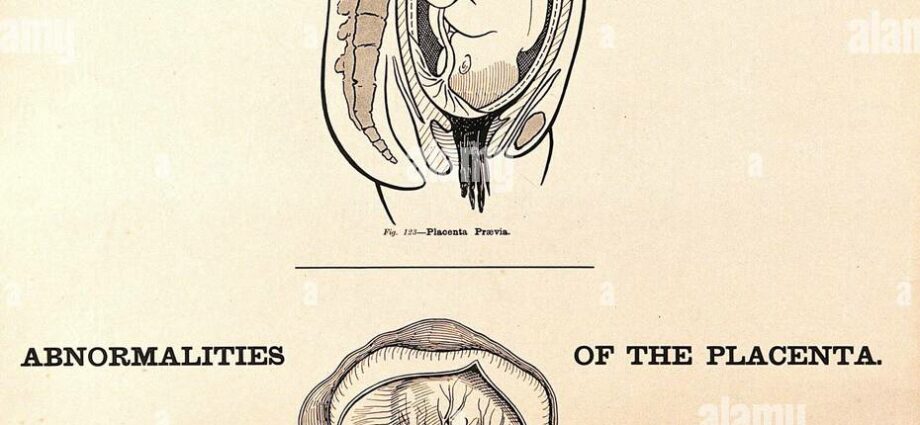
Until the 18th week of pregnancy, many placentas are positioned in the lower uterus, and this is not a problem. The vast majority “migrate” upwards as the uterus grows. A small percentage (1/200) is inserted near the cervix at the level of the lower segment (element which is formed in the 3rd trimester between the cervix and the body of the uterus). This is called a placenta previa. This position not only can make it difficult for the baby to come out, but is likely to cause bleeding when contractions occur. Complications depend on the distance of the placenta from the cervix. In rare cases, it completely covers the orifice and the birth can only be done by cesarean section.
What is an anterior placenta, posterior placenta, fundal placenta?
We speak of an anterior or posterior placenta depending on the position in which the placenta is located, whether it is behind or in front of the uterus. We also speak of fundal placenta when the placenta is located at the bottom of the uterus. This is only an indication of the position of the placenta; These terms do not necessarily refer to pathology or poor placental implantation.
When the placenta is infected
Maternal germs can reach the placenta in different ways. Through the blood, through the cervix or from the uterus itself. Depending on the date of infection, the consequences on pregnancy are variable (miscarriage, intrauterine growth retardation, premature delivery, neonatal involvement, etc.). The microbes can colonize the mass of the placenta or sit on the amniotic membranes. The ultrasound sometimes shows the placental infection, but it is not always obvious. After childbirth, the placenta will be sent to the laboratory to identify the germ with certainty.
When the placenta has a funny shape
At the end of pregnancy, the placenta (“pancake” in Latin) appears as a disc 20 cm in diameter and 35 mm thick. It weighs around 500-600 g. From time to time, it looks different. Instead of forming a single large mass, it is divided into two parts connected by the cord (placenta bi-partita). Other times, it’s a small placental lobe, which sits away from the main mass (aberrant cotyledon). Most often, these situations do not pose a problem.
When the placenta comes off too soon
When everything is going well, the placenta separates from the uterus at the time of delivery. When the phenomenon takes place before childbirth, a hematoma (blood bag) is created between the uterine wall and the placenta which causes an interruption of maternal-fetal exchanges. If the hematoma affects only a very small portion of the placenta, the risks are generally limited, and hospitalization with rest usually allows the pregnancy to continue normally. When the detachment involves the entire placenta, it is called a retro-placental hematoma. This complication, fortunately infrequent, can have serious consequences for mother and baby. The cause ? It is not well known, but there are contributing factors such as preeclampsia, smoking or abdominal shock. The first signs are usually characteristic: bleeding and sudden abdominal pain, very quickly followed by fetal distress. Once the diagnosis is made, no time to waste! The exit of the baby is essential.
Placenta accreta: when the placenta implants poorly
Normally, the placenta is inserted at the level of the uterine lining. This mechanism, formed very early in pregnancy, can unfold abnormally. This is the case when the adhesion of part or all of the placenta extends deeper than it should in the uterus. We then speak of placenta accreta. This fortunately rare implantation (1/2500 to 1/1000 pregnancies) can be complicated by hemorrhage at the time of delivery. This is because the placenta anchored in the wall of the uterus cannot come off normally. The treatment is complex, involving the entire medical team, and depends essentially on the extent of the bleeding.
When the placenta grows abnormally
This type of anomaly is rare, on the order of one pregnancy in 1. It is encountered in so-called molar pregnancies (or hydatidiform moles). The origin is chromosomal and occurs from fertilization. Bleeding at the beginning of pregnancy, severe nausea or vomiting, a soft uterus, larger than normal at term, can put the chip in the ear. The diagnosis is confirmed by ultrasound. Two types of hydatidiform moles exist. It may be a “complete” mole, in which there is never an embryo but a placenta which continues to grow into multiple cysts and takes on the appearance of a bunch of grapes, or of a partial mole in which an embryo can usually develop but abnormally, again with excessive placental growth. After the aspiration evacuation of the molar pregnancy, regular dosages of the pregnancy hormone (hCG) are prescribed for several months. Indeed, they are generally abnormally high in this type of disease, but must subsequently become negative. Sometimes a hydatidiform mole persists, or spreads to other organs. This situation requires more intense monitoring and treatment.