Contents
Medical treatments for urinary incontinence
It is important to see a doctor for symptoms that resemble urinary incontinence. Once the diagnosis is made, other healthcare professionals can offer helpful help. This may be an incontinence nurse consultant or a physiotherapist specializing in bladder rehabilitation. A list of professionals specializing in incontinence in Canada is available on the website of the Foundation for the support of incontinence (see Sites of interest). |
Treatment varies depending on the cause and severity of theurinary incontinence. If necessary, of course, the disease causing the incontinence should be treated, in addition to treating the symptoms.
Food
See the Prevention section for more information on foods to reduce or avoid.
Behavioral techniques
These techniques generally require the support of a physiotherapist or physiotherapist or a nurse. Some specialize in incontinence problems.
Kegel Exercises
This recognized practice improves the muscle tone pelvic floor (perineum). Both women and men can use it for stress or urge incontinence.
The exercices should be done regularly for several weeks to give a beneficial result. 40% to 75% of women who use it note an improvement in their control urinary1. In the case of men, this practice is mainly used after removal of the prostate (prostatectomy).
Notes. By strengthening the pelvic floor muscles, Kegel exercises can also improve the sexual pleasure.
How to practice Kegel exercises17,18 |
At the beginning, practice these exercises while lying on the back, the knees bent and slightly apart (with the width of the pelvis). Once mastered, start doing them sitting, then standing. — Contract pelvic floor muscles by maintaining the contraction for 5 to 10 seconds. (Make sure you are contracting the correct muscles! You should feel the contraction of the muscles around the vagina or penis, as if holding urine or stool. Caution: Do not squeeze the muscles of the stomach and buttocks.) — Breathe calmly during the contraction. — To release the contraction during 5 to 10 seconds. — Repeat from 12 to 20 times the cycle of contraction and relaxation. To be practiced 3 times a day, ideally in the morning, at noon and in the evening. For more information, see the information sheet produced by the Incontinence Foundation (section Sites of interest). |
biofeedback
Biofeedback can help women feel and control their pelvic floor muscle contractions better. This technique allows you to visualize on a computer screen the contraction and relaxation of the muscles during the practice of Kegel exercises. This visualization, which is done with the help of a sensor placed in the vagina, brings to consciousness, in a very precise way, the intensity of a contraction and its duration.
Bladder rehabilitation
This can be done in different ways, depending on the type ofurinary incontinence.
- One can delay urination. At first, when the urge to urinate is felt, we try to wait 10 minutes before relieving ourselves. This period is then increased to 20 minutes, the goal being to space urination by at least 2 hours (4 hours at most).
- In case of overflow incontinence, one can practice the exercise of the double drain. It consists of urinating, then trying again a few minutes later. It allows you to learn how to better empty your bladder in order to avoid an overflow of urine.
- One can adopt a fixed schedule. It’s about going to the bathroom at set times, rather than waiting until you want to urinate. The goal is to space urination by at least 2 hours, and 4 hours at most. This practice is very important and often effective in the elderly who have mobility problems.
- To control the urge to urinate, you can serelax taking a few deep breaths. You can also distract your attention by keeping busy: by reading, doing crosswords or washing dishes, for example.
electrostimulation
Electrical stimulation, or electrical stimulation, involves inserting an electrode into the vagina or anus to stimulate and tone the muscles of the pelvic floor. By combining this method with biofeedback, we can visualize muscle contractions on a computer screen. This then allows you to feel them better, and therefore to control them. This approach is usually reserved for people for whom behavioral techniques are ineffective.
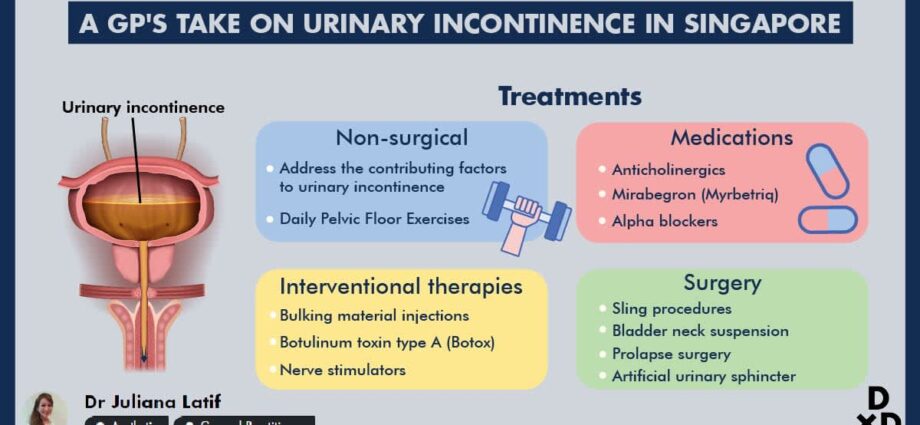
Medication
Some medicines help reduce the contractions of the bladder. They are therefore useful in case ofurgency urinary incontinence : oxybutynin (Oxybutynin® and Ditropan®, for example), flavoxate (Urispas®) and tolterodine (Detrol®). One of their side effects is dry mouth, which can cause patients to drink more. There are various ways to mitigate them. Discuss it with his doctor.
Local treatment with estrogen may help reduce symptoms for some women around the time of menopause. Estrogen is applied to the vagina in the form of eggs (eg, Vagifem®), rings (Estring®), or cream. The doses of hormones used are very small in the case of eggs and rings. They are slightly higher for cream, which sometimes requires a progestin (eg Provera®) to reduce the risks associated with long-term hormone therapy. For more information, see our Menopause sheet.
Other drugs can be used to treat the disease that causes urinary incontinence, for example, antibiotics for a urinary tract infection.
Miscellaneous devices and accessories
External devices
– Absorbent pads
– Diapers for adults
– Devices for collecting urine (men)
– Protective underwear
Internal devices
They are often used as a last resort.
– Catheter. It is a flexible and very thin tube connected to an outer bag. The tube is inserted into the urethra, which allows urine to pass into the bag. In some cases, patients can learn to insert and remove the catheter (3 or 4 times a day), which eliminates the need to carry a bag all the time.
– Pessary. The doctor inserts a rigid ring into the vagina to hold the bladder in place and prevent it from coming down. It is useful for women who have a descent of the bladder.
surgery
In many cases, surgery may be necessary. In women, it is most often used to maintain the bladder in place or to raise it when there has been descent of the bladder, by an intervention called cystopexie.
Can also :
– operate on a bladder tumor, uterine fibroid, urogenital fistula or prostate tumor;
– set up a device for suspending the neck of the bladder and the bladder in women;
– install an artificial urinary sphincter (especially in men);
– install a device that stimulates the sacral nerve (nerve located behind the sacrum).