Contents
Left ventricle
The left ventricle (ventricle: from the Latin ventriculus, meaning small belly) is a structure of the heart, serving as a point of passage for oxygenated blood to the body.
Anatomy of the left ventricle
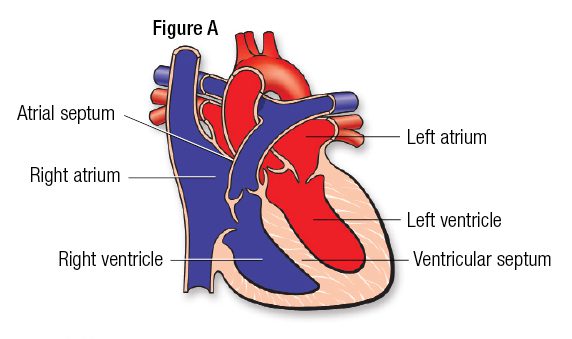
Position. Located at the level of the middle mediastinum within the thorax, the heart is divided into a right and a left part. Each of these parts has two chambers, an atrium and a ventricle (1). The left ventricle extends from the atrioventricular orifice (between the atrium and the ventricle) to the apex of the heart (2) .
Overall structure. The left ventricle forms a cavity bounded by (1):
- the interventicular septum, wall separating it from the right ventricle, on its middle part;
- the atrioventricular septum, a small wall separating it from the right atrium, on its middle and upper surface;
- the mitral valve, a valve separating it from the left atrium, on its upper surface;
- the aortic valve, valve separating it from the aorta, on its underside.
Internal structure. The left ventricle contains the fleshy trabeculae (fleshy columns), as well as the papillary muscles. These are connected to the mitral valve by the tendon cords (1).
Wall. The wall of the left ventricle is three times thicker than that of the right ventricle. It is made up of three layers (1):
- the endocardium, an inner layer made up of endothelial cells resting on connective tissue;
- the myocardium, a middle layer made up of striated muscle fibers;
- the pericardium, the outer layer enveloping the heart.
Vascularization. The left ventricle is supplied by the coronary vessels (1).
Function of the left ventricle
Blood path. Blood circulates in one direction through the heart and the blood system. The left atrium receives oxygen-rich blood from the pulmonary veins. This blood then passes through the mitral valve to reach the left ventricle. Within the latter, blood then passes through the aortic valve to reach the aorta and be distributed throughout the body (1).
Ventricular contraction. The passage of blood through the left ventricle follows the cardiac cycle. The latter is divided into two phases: systole, phase of tension and diastole, phase of relaxation (1) (3).
- Ventricular systole. Ventricular systole begins at the end of diastole, when the left ventricle is filled with blood. The mitral valve closes, causing pressure to increase in the left ventricle. The pressure exerted by the blood will lead to the contraction of the left ventricle, causing the aortic valve to open. The blood is then evacuated through the aorta. The left ventricle empties and the aortic valve closes.
- Ventricular diastole. Ventricular diastole begins at the end of systole, when the left ventricle is empty. The pressure within the ventricle lowers, causing the mitral valve to open. The left ventricle then fills with blood, coming from the left atrium.
Heart problems
Certain pathologies can affect the left ventricle and its structures. They can be the cause of irregular heartbeats, called cardiac arrhythmias, too fast beats, called tachycardias, or more simply chest pain.
Valvulopathie. It designates all the pathologies affecting the heart valves, in particular the grape valve and the aortic valve. The course of these pathologies can lead to a change in the structure of the heart with dilation of the left ventricle. Symptoms of these conditions can include a heart murmur, palpitations, or discomfort (4) (5).
Myocardial infarction. Also called heart attack, myocardial infarction corresponds to the destruction of part of the myocardium. The cause of this pathology is the obstruction of a coronary artery supplying the myocardium. Deprived of oxygen, myocardial cells die and degrade. This destruction results in a dysfunction of the cardiac contraction which can lead to the stop of the heart. A myocardial infarction is manifested in particular by abnormal heart rhythms or heart failure (6).
Angina pectoris. Also called angina, angina pectoris corresponds to an oppressive and deep pain in the thorax. It occurs most often during exertion but can also appear during periods of stress and more rarely at rest. The cause of this pain is an inadequate supply of oxygen to the myocardium. This is often due to pathologies affecting the coronary arteries, responsible for the irrigation of the myocardium (7).
Pericarditis. This pathology corresponds to inflammation of the pericardium. The causes can be varied but the origin is often a bacterial or viral infection. These inflammatory reactions can also cause fluid effusion leading to tamponade (1). The latter is characterized by compression of the heart by the liquid, preventing it from functioning normally.
Treatments
Medical treatment. Depending on the pathology diagnosed, different drugs may be prescribed such as anticoagulants, anti-aggregants, or even anti-ischemic agents.
Surgical treatment. Depending on the pathology diagnosed, a surgical intervention may be implemented. The fitting of a valve prosthesis can for example be carried out in certain cases of valve disease.
Examination of the left ventricle
Physical examination. First, a clinical examination is performed in order to study the heart rate in particular and to assess the symptoms perceived by the patient such as shortness of breath or palpitations.
Medical imaging exam. In order to establish or confirm a diagnosis, a cardiac ultrasound, or even a doppler ultrasound can be performed. They can be supplemented by a coronary angiography, a CT scan, a cardiac scintigraphy, or even an MRI.
Electrocardiogram. This test allows you to analyze the electrical activity of the heart.
Electrocardiogramme d’effort. This test makes it possible to analyze the electrical activity of the heart during physical exertion.
History
20th century South African surgeon Christiaan Barnard is famous for performing the first successful heart transplant. In 1967, he transplanted a heart from a young woman who died in a car accident to a man with coronary artery disease. This patient will survive after the operation but will succumb to pneumonia 18 days later (8). Since this first successful transplant, medical progress has continued as evidenced by recent experiments with transplants from an artificial heart.